Compassion is a key part of human connection. However, we don’t have an infinite well of compassion to pull from. Continuously pouring our time, energy, and empathy into others without having the time or support to replenish our own well can significantly impact our physical and mental health.
For people in helping professions, this may eventually lead to compassion fatigue (CF). While research shows that teachers and family caregivers are susceptible to CF, compassion fatigue primarily affects healthcare workers and emergency responders.
To better understand compassion fatigue and how medical professionals can preserve their mental and physical well-being in this emotionally demanding line of work, this article will break down the following:
- What is compassion fatigue?
- Different causes of compassion fatigue
- Signs and symptoms of CF
- How to avoid compassion fatigue
- Strategies for combating compassion fatigue
- What is the difference between CF, burnout, and secondary traumatic stress?
What Is Compassion Fatigue?
Compassion sits at the core of many helping professions. However, when you’re continually exposed to patient illness, trauma, or suffering, compassion fatigue can follow.
In essence, compassion fatigue is the emotional impact of traumatic stress—the condition occurs when burnout meets secondary traumatic stress. Physicians, critical care nurses, emergency responders, and disaster response behavioral health workers are among those most affected.
Along with physical and psychological symptoms, individuals experiencing CF may find that their productivity, interpersonal relationships, and morale suffer. Unfortunately, patient care can sometimes suffer as a result.
Compassion fatigue is considered the opposite of compassion satisfaction (CS). Medical professionals who have high CS experience a sense of fulfillment in their work and feel supported in the workplace. Greater CS can prevent the development of compassion fatigue.
Compassion Fatigue Definition
Compassion fatigue was originally defined similarly to burnout among healthcare professionals.
Eventually, the condition was separately distinguished as “a state of exhaustion and dysfunction — biologically, physically, and socially—as a result of prolonged exposure to compassion stress and all that it evokes.”
What Causes Compassion Fatigue?
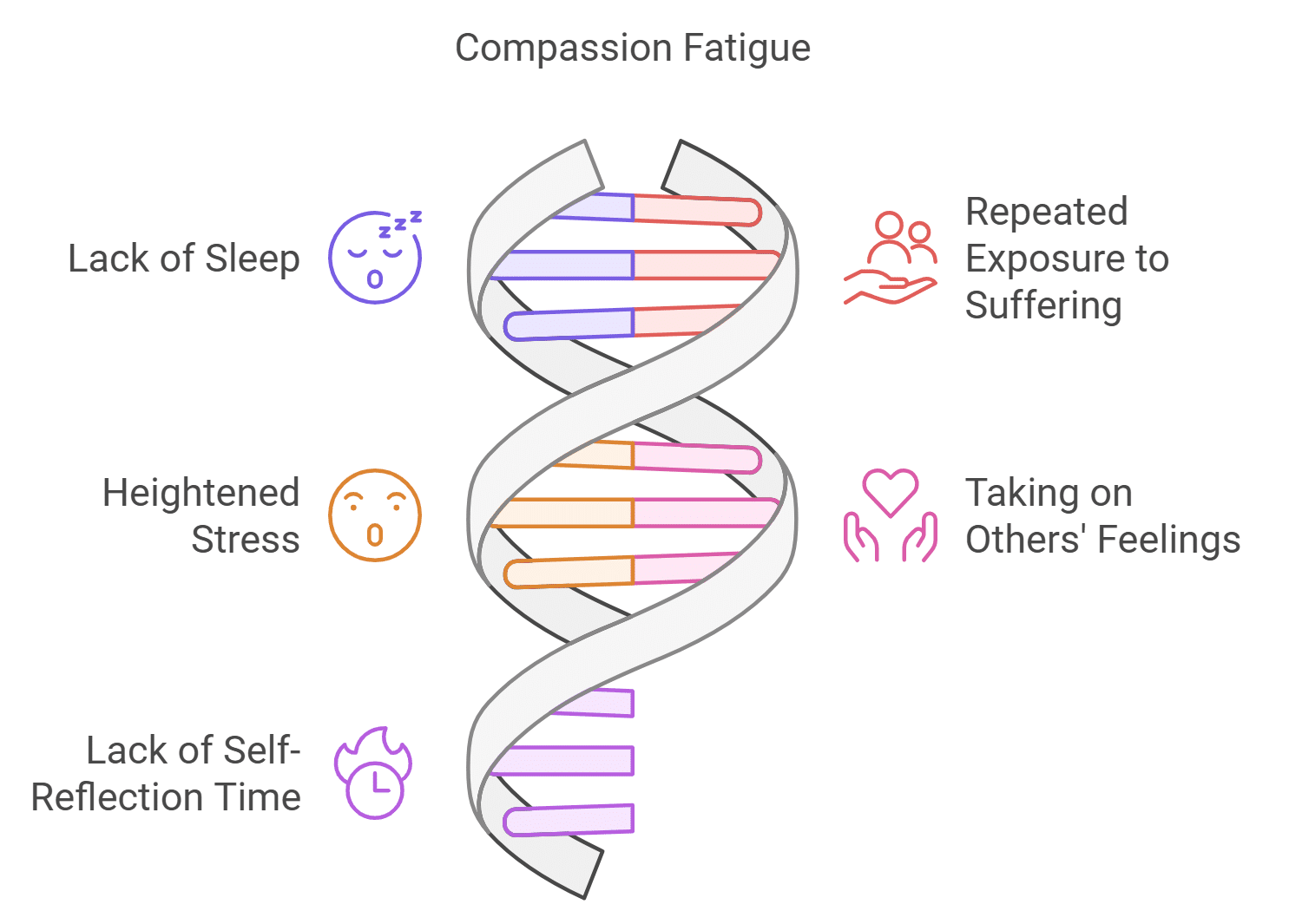
There is no single cause of compassion fatigue, and it doesn’t look the same in everyone experiencing it. However, there are some common causes that are responsible for many peoples’ CF:
- Lack of Sleep
Disaster responders work around the clock in the aftermath of a hurricane, fire, or other natural disaster. Long hours, noisy environments, and the psychological impacts of witnessing communities affected by trauma and devastation can negatively impact sleep.
A continuous lack of sleep can affect a person’s mental health, increasing the risk of compassion fatigue among disaster response workers.
- Repeated Exposure to Suffering
Healthcare professionals and emergency responders are regularly faced with illness, suffering, and death. Research shows that palliative or hospice care nurses may be particularly susceptible to compassion fatigue.
The nature of their work focuses on improving the quality of life for patients who may be in pain or near death, which can wear on a person’s physical, psychological, and spiritual well-being.
- Heightened Stress
Working in high-pressure environments can increase stress, which can build to the point of CF, particularly among healthcare professionals who hold themselves to high personal standards. Prolonged exposure to stressors can also cause physical symptoms, including nausea, headaches, and chest pain.
- Taking on the Feelings of Others
The fine line between compassion and overinvolvement in patient care can be difficult to walk. Empathy may be a pillar of many helping professions, but personally taking on the suffering of a patient can lead to feelings of helplessness and emotional exhaustion.
For disaster workers, guilt may also surface in response to being unable to rescue someone or for having survived a traumatic event themselves, all of which can fuel compassion fatigue.
- Lack of Time for Self-Reflection
It’s a natural human instinct to practice avoidance in order to preserve one’s psychological well-being. Employers who actively create a supportive work environment for healthcare professionals to reflect on their feelings and responses to stress help maintain patient standards of care in the process. Taking these precautionary measures also reduces emotional fatigue among their employees.
- Job Demands
Work overload, staffing shortages, and administrative and clinical demands of the job can leave doctors and other medical professionals emotionally spent. Healthcare facilities that lack financial resources can place additional strain on their employees, further contributing to compassion fatigue.
Signs and Symptoms of Compassion Fatigue
Compassion fatigue shows up differently in each person. However, some common signs of compassion fatigue among those in helping professions include:
- Exhaustion
- Trouble sleeping
- Cynicism or reduced empathy
- Repeatedly calling out of work
- Intrusive or ruminating thoughts
- Lack of connection with co-workers
- Increased alcohol or substance use
- A sense of powerlessness in the workplace
- Difficulty concentrating or making decisions
- Feelings of anxiety, overwhelm, or irritability
Individuals may also experience physical symptoms of compassion fatigue, such as:
- Chest pain
- Headaches
- Gastrointestinal discomfort
- Feelings of general illness or weakness
How to Combat Compassion Fatigue
Strategies to effectively combat compassion fatigue can be implemented by healthcare professionals as well as the larger organizations that employ them. To prevent CF, we must address our individual needs as well as larger systemic factors. Here’s how healthcare workers can reduce compassion fatigue and maintain their mental health:
- Lifestyle Changes to Maintain Physical Health: Low-impact to moderate-intensity exercise—like swimming, walking, or yoga—on a weekly basis can help keep stress levels in check. Getting seven to nine hours of sleep nightly, staying adequately hydrated, and eating nutritious foods that support our health and energy levels can also keep compassion fatigue at bay.
- Grounding Techniques & Mindfulness Practices: Meditation, journaling, visualization techniques, and breathing exercises are practices that can calm the nervous system and relax the body.
- Reach Out to Your Support Network: Being in a community with friends, family members, or co-workers can help healthcare professionals process their emotions and avoid self-isolation.
- Seek Support in the Workplace: Ask for help within your organization if you’re feeling emotionally depleted. Managers can support their employees by offering positive feedback, scheduling shifts far enough apart to allow for rest, and creating a safe space for healthcare workers to communicate their needs.
- Therapeutic Support: While self-care is an important preventative tool, seeking therapeutic support from a mental health professional is the best way to address the psychological impacts of compassion fatigue.
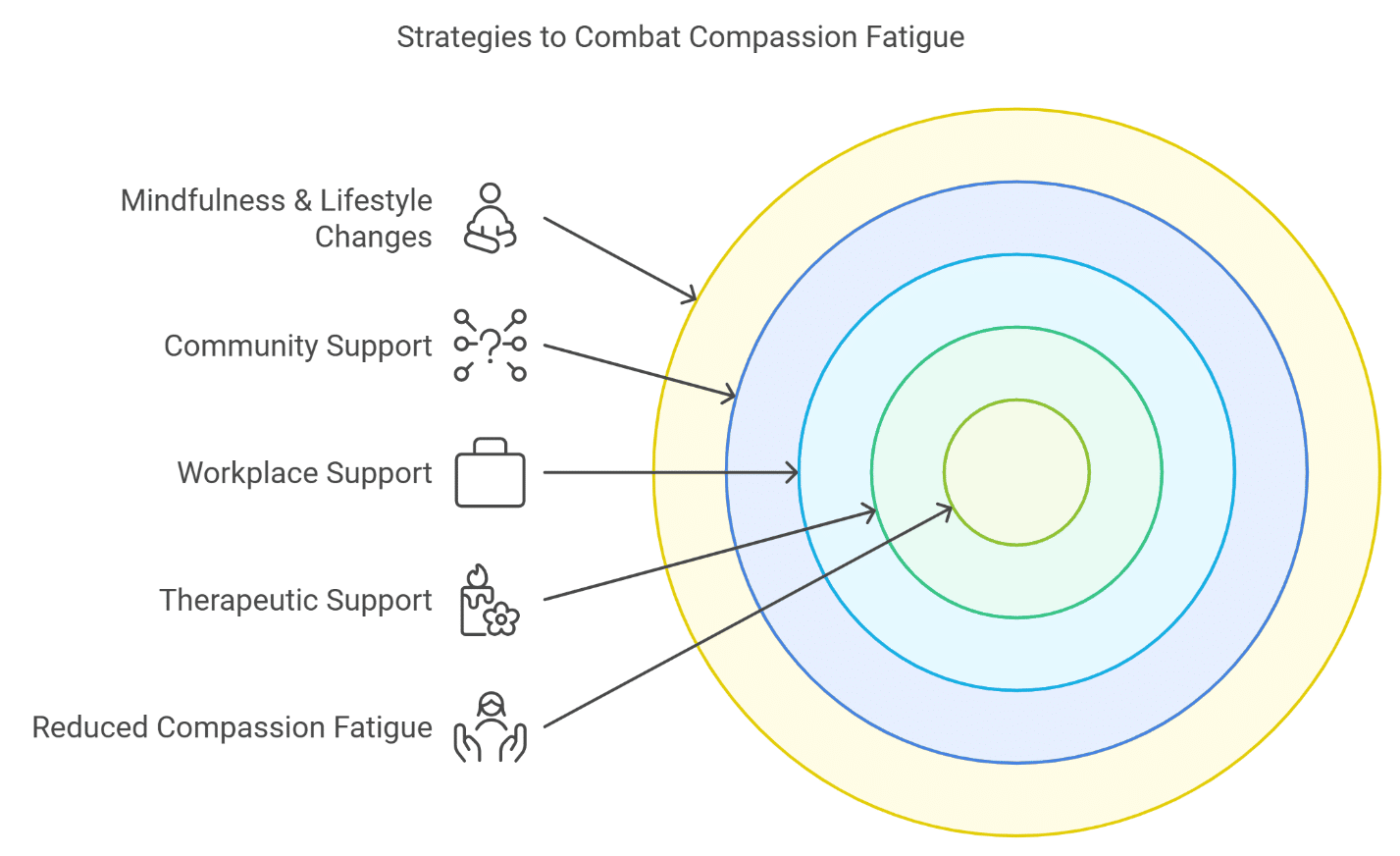
At Mission Connection Healthcare, our experts use a variety of evidence-based therapeutic approaches to treat mental health holistically.
Healthcare workers experiencing compassion fatigue may benefit from services such as Eye
Movement Desensitization and Reprocessing (EMDR) therapy for processing trauma; Dialectical Behavior Therapy (DBT) for emotion regulation; or Emotion-Focused Therapy (EFT) aimed at building emotional resilience.
Get Support For Compassion Fatigue Today
If you’re experiencing signs of compassion fatigue, there is no reason to feel guilt or shame. Whether it’s the demands of your job, continuous exposure to trauma, or taking on the emotions of others, compassion fatigue is a real risk in many helping professions. So, you’re not alone.
In addition to prioritizing the well-being of your patients, make time to replenish your own emotional well. Your well-being is equally as important.
Reach out to Mission Connection Healthcare today through our confidential hotline at 866-753-5791 or get started with our online mental health assessments to determine which therapeutic approach may be right for you.
Compassion Fatigue FAQs
+ Compassion fatigue vs. burnout: what’s the difference?
For those in helping professions, compassion fatigue and burnout can look a lot alike. While they do share similar symptoms, burnout is characterized by feelings of exhaustion and overwhelm while compassion fatigue is a state of burnout mixed with trauma-related stress.
+ How to avoid compassion fatigue
You can avoid compassion fatigue by using a variety of self-care strategies and mental health resources. Maintaining your physical health with regular exercise, adequate sleep, and a healthy diet can all reduce the risk of compassion fatigue. Additional self-care strategies include meditation, breathing exercises, and reaching out to others.
+ Which two conditions are often present in someone with compassion fatigue?
Burnout and secondary traumatic stress are the two mental health conditions that make up compassion fatigue. People with burnout experience exhaustion, frustration, and helplessness in relation to their work.
Secondary traumatic stress is the stress a healthcare worker takes on from continuous exposure to the trauma of others. This can often lead to fear that they themselves are experiencing the same trauma. Secondary traumatic stress is considered the more severe of the two parts of compassion fatigue.
References
Alharbi, J., Jackson, D., & Usher, K. (2019). Compassion fatigue in critical care nurses. An integrative review of the literature. Saudi medical journal, 40(11), 1087–1097. https://doi.org/10.15537/smj.2019.11.24569
Cross L. A. (2019). Compassion Fatigue in Palliative Care Nursing: A Concept Analysis. Journal of hospice and palliative nursing : JHPN : the official journal of the Hospice and Palliative Nurses Association, 21(1), 21–28. https://doi.org/10.1097/NJH.0000000000000477
Day, J. R., Anderson, R. A., & Davis, L. L. (2014). Compassion fatigue in adult daughter caregivers of a parent with dementia. Issues in mental health nursing, 35(10), 796–804.
https://doi.org/10.3109/01612840.2014.917133
Kase, S.M., Gribben, J.L., Guttmann, K.F. et al. Compassion fatigue, burnout, and compassion satisfaction in pediatric subspecialists during the SARS-CoV-2 pandemic. Pediatr Res 91, 143–148 (2022). https://doi.org/10.1038/s41390-021-01635-y
Ormiston, H. E., Nygaard, M. A., & Apgar, S. (2022). A Systematic Review of Secondary Traumatic Stress and Compassion Fatigue in Teachers. School mental health, 14(4), 802–817. https://doi.org/10.1007/s12310-022-09525-2
SAMHSA (2014). Tips for Disaster Responders: UNDERSTANDING COMPASSION FATIGUE. U.S. Department of Health & Human Services.
https://store.samhsa.gov/sites/default/files/sma14-4869.pdf
SAMHSA (2020). Tips for Healthcare Professionals: Coping with Stress and Compassion Fatigue. U.S. Department of Health & Human Services. https://store.samhsa.gov/sites/default/files/PEP20-01-01-016_508.pdf
SAMHSA (2024). Compassion Fatigue and Self-care Resources for Crisis Counselors. U.S.
Department of Health & Human Services.


