OBGYN Referrals for Perinatal Mental Health Care

Expecting a baby brings enormous change, not just physically, but emotionally and psychologically as well. In fact, research shows that many women experience mental health challenges during and after pregnancy.¹ From anxiety and depression to trauma resurfacing, perinatal mental health concerns are common. But they’re also treatable and deeply important to address.
Research shows that around 20% of obstetrician-gynecologists (OB-GYNs) screen for anxiety when treating pregnant women.² Others may notice signs of depression or anxiety and refer patients to mental healthcare facilities for help. 10% of the global population of pregnant women experience a mental health disorder with around 12% suffering from depression and 13% experiencing anxiety.³ Many women experience both.
At Mission Connection, we help pregnant and postpartum women access therapy, medication management, and supportive services tailored to their unique stage of life.
This guide will walk you through the following aspects of OB-GYN referrals for mental health:
- The role of an OB-GYN in the mental health of pregnant women
- When and why mental health referrals happen in perinatal care
- Types of OB-GYN support for mental health
- How OB-GYNs connect patients with perinatal mental health providers
- Accessing mental health resources without insurance
- How to find the right mental health support during and after pregnancy
The OB-GYN’s Role in Mental Health During Pregnancy
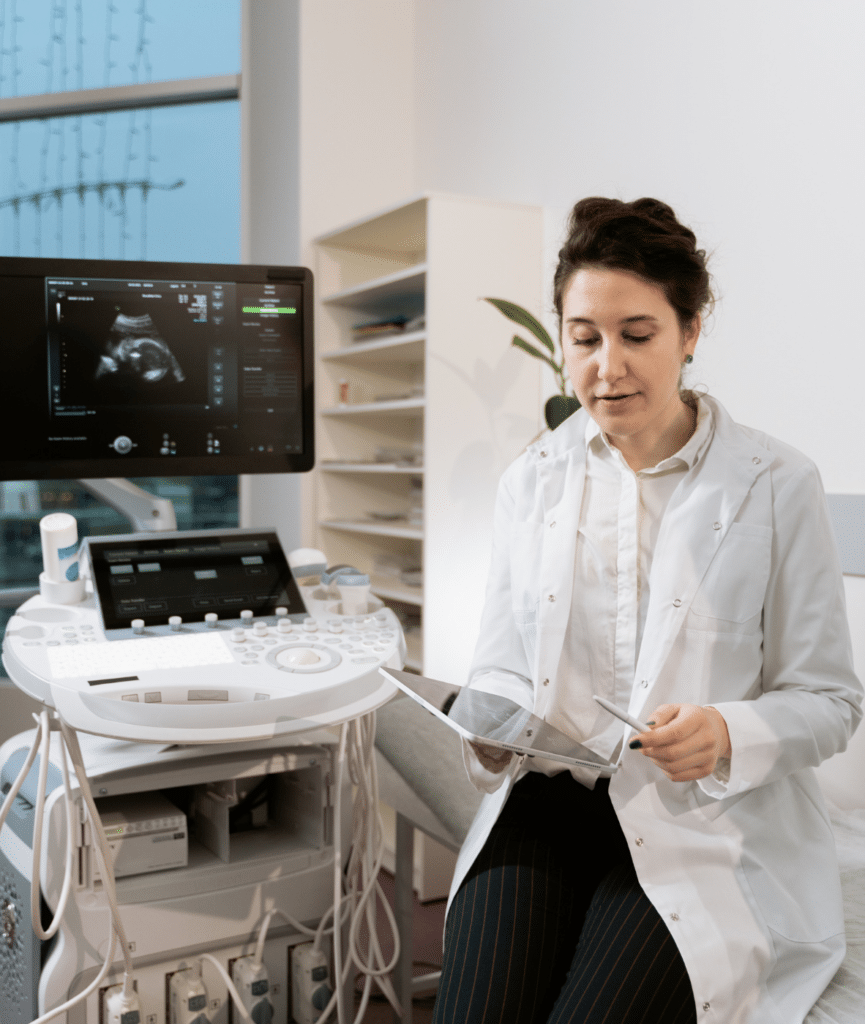
OB-GYNs often serve as the first point of contact for pregnancy and mental health referrals, helping expectant mothers connect with the right support at a crucial time. Not just physically, but emotionally, too.
Common mental health concerns that some pregnant women face include:
Many women find themselves admitting feelings of worry, sadness, anger, or irritability in the exam room before they’ve told anyone else. This is where OB-GYN referrals for perinatal mental health care often begin.
Depending on symptoms, OB-GYN mental health consultations are often a stepping stone to mental health treatment for expecting mothers, of which there are many options. Let’s explore some below:
Cognitive Behavioral Therapy (CBT)
CBT is one of the most commonly recommended therapies for women looking for perinatal care and mental health services. It helps reduce anxiety and depressive symptoms by breaking down distorted thinking patterns. CBT is widely supported in the research literature as an effective treatment for perinatal mood and anxiety disorders, including postpartum depression.⁴
Interpersonal Therapy (IPT)
This approach focuses on helping a person understand and manage strained relationships, grief, and social transitions. Many pregnant patients feel isolated or overwhelmed by shifting roles and circumstances. IPT is one of the few therapies specifically validated for perinatal depression in clinical studies.⁵
Mindfulness-Based Cognitive Therapy (MBCT)
When stress feels chronic, OB-GYN referrals for perinatal mental health might point to MBCT. MBCT helps people become aware of emotional patterns without reacting automatically. Randomized controlled trials show that MBCT can reduce relapse in depression during pregnancy.⁶
Compassion-Focused Therapy (CFT)
For patients carrying trauma or deep shame, CFT builds inner safety through guided compassion work. It’s especially relevant for pregnant women with a history of abuse or chronic self-blame. Research suggests CFT changes how the brain processes threat and safety, helping expectant and new moms parent from a place of security.⁷
Peer-Based Support Groups
Peer support groups are about co-regulation and healing together, and they form part of the treatments offered by perinatal mental health care providers. Social support (group support provided by peers with a shared lived experience) has been shown to decrease postpartum symptom severity and foster stronger emotional bonds between parent and child.⁸
Medication Referral
In more severe cases, medication may be necessary. An OB-GYN may consult with a perinatal psychiatrist to weigh options, ensuring any medication is safe during pregnancy. Antidepressants like sertraline are sometimes prescribed after referrals for postpartum depression care. However, these medications are closely monitored throughout.
Referrals from an OB-GYN are often the turning point for pregnant and new moms. When someone is struggling, early recognition and direction toward proper care can alter the entire course of pregnancy and postpartum adjustment.
When and Why Mental Health Referrals Happen in Perinatal Care
The U.S. Preventive Services Task Force, the American College of Obstetricians and Gynecologists, and the American Academy of Pediatrics all recommend screening for depression during the perinatal period.⁹
OB-GYN referrals for perinatal mental health during pregnancy don’t just happen when someone directly tells a medical professional that they’re feeling low. Sometimes patients aren’t sure what they’re experiencing and may end up visiting their OB-GYN when they should be seeing a mental health care provider. Connecting with perinatal mental health professionals is usually the next step, after a referral.
The signs of depression and anxiety can show up during routine visits. The patient may have an unusually flat tone or seem emotionally disconnected. She may also mention that she’s not sleeping well or is struggling with feelings of panic. These can be signs that something deeper is going on.
Referrals are also often made if the patient has:
- A history of anxiety or trauma
- Been feeling numb recently
- Feelings of overwhelm
- Irritability
Sometimes it’s hearing about these moments or noticing them that spurs a healthcare provider to take action, like a comment about not feeling excited or being afraid to go home.
OB-GYN referrals for perinatal mental health are also made when outside stressors become too much like conflict in relationships, unstable housing, financial strain, or lack of social support. These factors raise the risk of perinatal mood disorders and noticing them early can make all the difference.
The purpose of a referral is to offer support before things escalate. When mental health is addressed early in pregnancy, it strengthens the foundation for recovery, parenting, and postpartum well-being.
How to Access Perinatal Mental Health Care Through an OB-GYN Referral
If a woman says she’s not coping, the next step is usually a referral. Some clinics offer in-house therapy while others refer out to a list of mental health providers they trust. In urgent cases, like possible postpartum psychosis, a direct psychiatric consultation might happen the same day.
The process depends on several things like where the person lives, what insurance covers, and how quickly care is needed. But OB-GYNs often act as the bridge between physical care and emotional support, especially when someone doesn’t know where else to begin.
Mental health professionals and OB-GYNs often share information – with the patient’s consent – to monitor symptoms, adjust treatment plans, and ensure any medication prescribed is safe during pregnancy. Supporting mental health during pregnancy may look like:
- Joint check-ins or updates between providers
- Sharing screening results or patient progress notes
- Aligning medication plans, especially if antidepressants or anti-anxiety medications are considered
Research has shown that collaborative perinatal care leads to better outcomes.¹⁰ It reduces symptom severity, improves birth outcomes, and helps women feel more supported throughout their pregnancies.
The team at Mission Connection supports a collaborative approach by assisting pregnant women and their healthcare providers create a cohesive treatment plan. Our team works alongside OB-GYNs to ensure timely OB-GYN referrals for perinatal mental health, therapeutic interventions, and follow-up support are all part of a woman’s mental health care during pregnancy.
Accessing Mental Health Resources Without Insurance
Getting mental health support while pregnant is important, even if you don’t have insurance. It might take a few extra steps, but help is still available, and often more affordable than expected.
Local Clinics That Offer Free or Low-Cost Care
A good place to start is with the local community health centers. Many of these facilities may offer counseling for pregnant women, even without insurance. Some might even use a sliding scale based on your income or be able to direct you toward free mental health resources for expecting mothers. Federally qualified health centers (FQHCs) are a good place to look because they’re designed to help people with little or no coverage.
What Hospitals Can Offer
Even if you’re uninsured, hospitals and OB clinics may be able to help. Some have social workers on staff who can walk you through available options. If your symptoms are severe like panic attacks, intrusive thoughts, or trouble functioning, you can still go to the emergency room. Hospitals cannot deny care based on insurance status.
Finding Support Online or Through Nonprofits
Some therapy platforms now offer lower-cost services or short-term free access. Postpartum Support International and similar organizations can connect you to therapists, support groups, or crisis lines that are open to people without insurance. Many of these services are designed with pregnant women in mind.
At Mission Connection, we help people find mental health support, even if they’re uninsured. Whether you need someone to talk to or you’re looking for longer-term therapy, we’ll help you figure out the next step.
What to Expect From a Perinatal Mental Health Referral
If you’re struggling with symptoms like anxiety, persistent sadness, or emotional numbness, your provider may suggest connecting with a perinatal mental health specialist.
1. An Intake Appointment
After receiving OB-GYN referrals for perinatal mental health, most expecting mothers meet with a licensed therapist or counselor trained in maternal mental health. This first session is typically an intake appointment, where you’ll talk about your emotional state, personal history, and any challenges you’re facing. It’s not a test, just a way to understand what kind of care will help most.
2. Tailored Support Plans
After your first session, your therapist helps shape a plan that fits your situation. That might involve meeting weekly, joining a small peer group, or connecting with a psychiatrist to talk through medication options. Every plan is different, shaped by how you’re feeling, what’s happening in your life, and what kind of support feels manageable right now.
3. Ongoing Collaboration
In most instances, the OB-GYN will continue being involved in your care. In some cases, the prenatal team and mental health care provider will be in contact with each other. It’s not just about managing symptoms. It’s about making sure your emotional and physical health are both being looked after, side by side. This kind of steady support can make all the difference, both during pregnancy and after birth.
Contact Mission Connection for Perinatal Care and Mental Health Services
When it comes to helping expecting mothers, the Mission Connection team is dedicated to integrated care. We assist moms-to-be work through the complex emotions that come with pregnancy. Each of our qualified therapists knows just how layered pregnancy can be. We will work alongside OB-GYNs to make sure your mental health is part of the conversation from early on.
If you need help finding mental health care during pregnancy, you can reach out with questions at any time – no referrals needed. You’re also welcome to discuss pregnancy and mental wellness referrals with our team. Whether it’s one conversation or advice on accessing perinatal mental health care, we’re here to help you feel steadier in your body and mind.
Contact us to learn more about your perinatal mental health options today.

References
- Li, X., Laplante, D. P., Paquin, V., Lafortune, S., Elgbeili, G., & King, S. (2022). Effectiveness of cognitive behavioral therapy for perinatal maternal depression, anxiety and stress: A systematic review and meta-analysis of randomized controlled trials. Clinical Psychology Review, 92, 102129. https://www.sciencedirect.com/science/article/abs/pii/S0272735822000149
- Modak, A., Ronghe, V., Gomase, K. P., Mahakalkar, M. G., & Taksande, V. (2023). A comprehensive review of motherhood and mental health: Postpartum mood disorders in focus. Cureus, 15(9), e46209. https://pmc.ncbi.nlm.nih.gov/articles/PMC10613459/
- Shortis, E., Warrington, D., & Whittaker, P. (2020). The efficacy of cognitive behavioral therapy for the treatment of antenatal depression: A systematic review. Journal of Affective Disorders, 272, 485–495. https://pubmed.ncbi.nlm.nih.gov/32553392/
- Baattaiah, B. A., Alharbi, M. D., Babteen, N. M., Al-Maqbool, H. M., Babgi, F. A., & Albatati, A. A. (2023). The relationship between fatigue, sleep quality, resilience, and the risk of postpartum depression: An emphasis on maternal mental health. BMC Psychology, 11(1), 10. https://bmcpsychology.biomedcentral.com/articles/10.1186/s40359-023-01043-3#:~:text=Their%20results%20suggest%20that%20poor,which%20PPD%20symptoms%20were%20studied
- Zappas, M. P., Becker, K., & Walton-Moss, B. (2021). Postpartum anxiety. The Journal for Nurse Practitioners, 17(1), 60–64. https://www.sciencedirect.com/science/article/abs/pii/S1555415520304529
- Institute for Quality and Efficiency in Health Care. (2022). In brief: Cognitive behavioral therapy (CBT).https://www.ncbi.nlm.nih.gov/books/NBK279297/#:~:text=For%20example%2C%20you%20can%20learn,letting%20your%20anxiety%20overwhelm%20you
- Horáková, A., Němcová, H., Mohr, P., & Sebela, A. (2022). Structural, functional, and metabolic signatures of postpartum depression: A systematic review. Frontiers in Psychiatry, 13, 1044995. https://pmc.ncbi.nlm.nih.gov/articles/PMC9709336/#:~:text=Wonch%20et%20al
- Shou, H., Yang, Z., Satterthwaite, T. D., Cook, P. A., Bruce, S. E., Shinohara, R. T., Rosenberg, B., & Sheline, Y. I. (2017). Cognitive behavioral therapy increases amygdala connectivity with the cognitive control network in both MDD and PTSD. NeuroImage: Clinical, 14, 464–470. https://pmc.ncbi.nlm.nih.gov/articles/PMC5331144/#:~:text=Conclusion,in%20both%20MDD%20and%20PTSD
- Pan, J., Luo, W., Zhang, H., Wang, Y., Lu, H., Wang, C., Li, C., Fu, L., Hu, Y., Li, Y., & Shen, M. (2025). The Effects of Online Cognitive Behavioral Therapy on Postpartum Depression: A Systematic Review and Meta-Analysis. Healthcare, 13(7), 696. https://doi.org/10.3390/healthcare13070696
- Guille, C., Newman, R., Fryml, L. D., Lifton, C. K., & Epperson, C. N. (2013). Management of postpartum depression. Journal of Midwifery & Women’s Health, 58(6), 643–653. https://doi.org/10.1111/jmwh.12104
- Pedro, L., Branquinho, M., Canavarro, M. C., & Fonseca, A. (2019). Self-criticism, negative automatic thoughts and postpartum depressive symptoms: the buffering effect of self-compassion. Journal of Reproductive and Infant Psychology, 37(5), 539–553. https://doi.org/10.1080/02646838.2019.1597969
- Branquinho, M., Canavarro, M. C., & Fonseca, A. (2022). A blended cognitive–behavioral intervention for the treatment of postpartum depression: A case study. Clinical Case Studies, 21(5), 438–456. https://doi.org/10.1177/15346501221082616