Depression in Women: A Complete Guide

Major depressive disorder, or “clinical depression,” is a diagnosable condition which causes persistent sadness or hopelessness that affects everyday life. It’s also a complicated illness, which can be caused by multiple factors, such as genetics, biology, and previous experiences.
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), to meet the criteria for depression, someone needs to have five out of nine depression symptoms daily, for a minimum of two weeks. In other words, depression in women symptoms last for two weeks at minimum – and can persist for much longer if left untreated.
If you’re concerned about the symptoms of depression in yourself or someone you care about, support and advice are available. Depression can feel isolating, but you don’t have to cope with it alone. This article can help by highlighting how and why depression affects women differently than men. It covers…
Whether depression is common in women – and why- Depression in women symptoms
- How stress can lead to depression in women
- Hormonal depression in women
- Depression during pregnancy
- Premenstrual dysphoric disorder
- The link between menopause and depression
- Best therapy treatment for women’s depression

Key Takeaways
- Women are about twice as likely as men to experience depression at some point in their lives.
- Hormonal changes (e.g., menstrual cycle, pregnancy, postpartum, menopause) can contribute to women's increased vulnerability to depression.
- Psychological and social pressures — such as stress, caregiving, relationship dynamics, and life demands — often combine with biological factors to increase risk.
- Symptoms of depression in women can include persistent sadness, fatigue, sleep or appetite changes, mood swings, difficulty concentrating, and loss of interest or pleasure in daily activities.
- Effective support involves holistic, personalized care — addressing emotional, biological, social, and lifestyle factors together.
Table of Contents
Is Depression Common in Women?
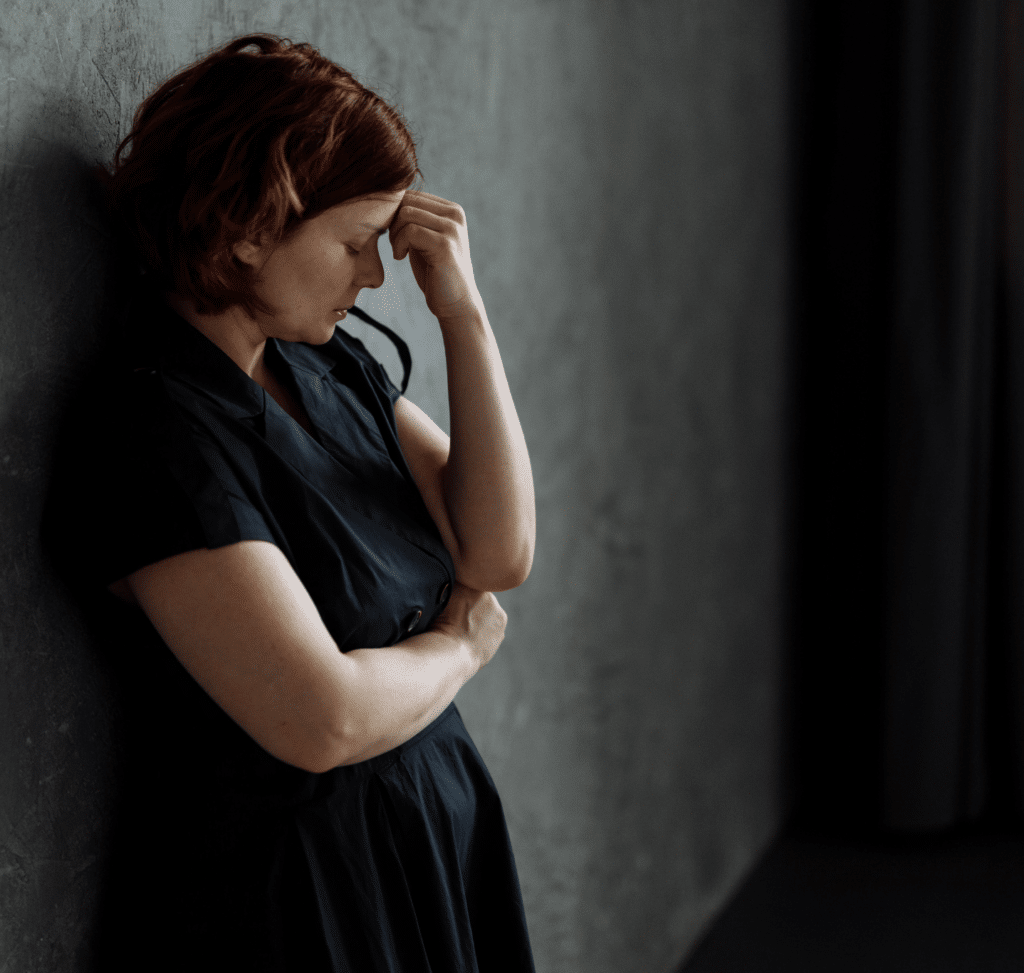
Instead of managing their low moods in healthy ways, such as reporting them to a doctor or mental health professional, women may cope by denying that the problem exists and isolating themselves from loved ones.
This denial of depression’s symptoms can leave women prone to co-occurring mental health conditions, such as anxiety, self-harm, eating disorders, and post-traumatic stress disorder (PTSD). However, this doesn’t have to be the case.
Depression is a treatable condition, and with the right treatment, understanding, and support, women can recover from the effects of depression. A good place to start is building awareness of the signs of depression in women.
Depression in Women Symptoms
Mental illness doesn’t typically come out of nowhere – there are usually signs that someone may be struggling to cope. Even if the person doesn’t immediately recognize these signs, or is denying their existence, a loved one, such as a family or friend, may be able to spot that something is “off.”
If you notice a change in how you’re thinking, feeling, or acting, these changes may indicate something serious such as depression. Alternatively, you may notice a shift in how someone else is behaving or talking. The key thing is, the earlier depression in women symptoms can be detected, the better the outlook for their well-being. Treatment can ensure that mental health conditions such as depression can be managed and that the effects on someone’s emotional and physical health are less severe.
Depression in women symptoms include:
- Persistent sadness or hopelessness about the future
- Feeling very tired or low in energy
- Loss of pleasure in activities that were once enjoyed
- Disrupted sleep
- Changes in appetite or weight (loss or gain)
- Feelings of excessive guilt or low self-worth
- Poor concentration,
- Self-harming behaviours
- Heightened sensitivity to smells, sounds, and touch, causing avoidance of stimuli
- Nervousness, fear, and/or suspicion of others
- Thoughts about death
Everyone is unique, so while some women may only experience a couple of these signs of depression, others may encounter a lot of them. However, if depression in women symptoms are affecting your life on a daily basis, for two weeks or longer, then it may be important to reach out for support. A doctor, mental health professional, or mental health care provider can discuss your concerns with you and provide avenues for treatment.
It can also help to understand the potential causes of depression in women, which we discuss in more detail next.
Stress and Depression in Women
Depression is one of the most common mental health conditions in women, altering mood, behaviors, and how they think about themselves. Plus, it can be triggered at any stage of life by stressful events.
Short-term stress can be beneficial as it gives you the energy to act and change a situation for the positive. However, long-term stress in another story entirely; it can negatively impact physical and mental health – and even contribute to depression.
To understand how to best treat depression, researchers have been exploring how men and women cope with stress and depression differently. Based on findings, it’s now recognized that long-term stress or upset in women can manifest as depression, self-harm, and eating disorders. This may be because of the following reasons.
1. Women May Internalize Their Emotions:
Women are more likely to internalize their emotions as self-blame and guilt. Therefore, long term stress may lead to issues such as poor self-esteem, sleep problems, and persistent sadness. In contrast, men may externalize their stress, leading them to become more angry or irritable.
2. Stress Can Affect Women Differently During Unique Life Stages:
Different forms of stress during unique stages of life can present certain challenges. For instance, the events that cause you to worry as a 20–year-old won’t necessarily be the same as those that induce stress at 60.
3. Societal and Internal Expectations Can Affect Depression in Women:
Another factor at play in the relationship between stress and depression is that women often take on many diverse roles, such as partner, mother, friend, carer, business owner, and so on. For example, women often take on the role of caretakers in families, so they do a lot of the emotional heavy lifting – which can increase stress. In fact, evidence suggests that women are more negatively impacted than men by the pressure of caregiving responsibilities. This impact can result in them experiencing symptoms of low mood or even depression.4
In addition to these reasons, some experts believe that the social idea of gender roles has led to men being expected to be the breadwinner, and to be resilient in times of stress. The notions of asking for help, accessing healthcare, and reporting symptoms of stress are seen as more “feminine” traits. Meaning that greater numbers of women report symptoms of depression and can access more timely mental health support than men. This might go some way towards explaining why three times as many men as women die by suicide – but this could also come down to their choice of methods.5
Hormonal Depression in Women
Research shows that mood swings are linked to hormonal changes during the menstrual cycle. This is because the neurochemistry in the brain is altered during the menstrual cycle, giving rise to fluctuations in mood.
A growing body of literature talks about how the female brain is very changeable during the menstrual cycle. The limbic system is the part of the brain responsible for regulating emotions and behaviour, and hormonal changes during menstruation often affect this system. Therefore, these changes can increase women’s risk of experiencing anxiety and depression.6
Sex hormones and stress can also interact to increase a woman’s risk for anxiety and depression. This is because, where estrogen usually has a protective element helping to regulate emotions, high levels of stress reduce the functioning of estrogen, making women more vulnerable to anxiety.6
Later in life, during menopause, women experience a sharp decline in estrogen levels, which is also known to be a cause of increased anxiety.
Depression During Pregnancy: Perinatal Depression
Perinatal depression can begin in pregnancy or emerge after the baby is born (postpartum). An estimated one in seven women experiences perinatal depression.7
Further, there are also psychosocial factors that can contribute to depression during pregnancy. A transition in identity, such as becoming a new mother, can cause some to feel highly anxious or depressed if they perceive a lack of support. Financial stress during pregnancy can also be a big factor.
Additionally, women from certain ethnic backgrounds may face barriers when it comes to accessing mental health services.
Depression After Pregnancy: Postpartum Depression
When you become a new mom, there can be an expectation that you will bond instantly and the transition will be seamless as you adjust to the role of mother. Unfortunately, this is often not the case.
While bringing a new human being into the world can be a joy-filled experience, it can also tip women into a spiral of low mood and postpartum depression. Many new moms feel overwhelmed with the major changes that touch every aspect of their life, and it is common for them to feel highly stressed. In fact, 85% of new mothers experience the “baby blues” in the first few weeks.
Tearfulness, difficulties sleeping, changes in appetite, anxiety, and shifts in thought patterns are all signs of the baby blues, which can make even the simplest task seem impossible. The majority of mothers who experience the baby blues find it to be a short-term phase that they get through – the symptoms are usually not severe and quickly subside.
However, as many as 20% of women in the US experience postpartum depression, so if any of the following symptoms persist, it is important that you do not struggle alone and you talk to your doctor or pediatrician.8
The signs of postpartum depression are:
Anxiety
- Persistent sadness
- Frustration or overwhelm
- Irritability
- Diminished interest in usual day-to-day activities
Premenstrual Dysphoric Disorder (PMDD) and Depression
Symptoms of premenstrual dysphoric disorder (PMDD) usually start a week before menstruation and can last a few days after your period ends. Those at increased risk of PMDD and depression usually have a family history of premenstrual syndrome (PMS) or PMDD.
The following are signs of PMDD:
- Depressed mood, sadness, hopelessness, or worthlessness
- Mood swings
- Increased anxiety
- Increased sensitivity to rejection
- Decreased interest in normal activities
- Difficulties concentrating
- Lack of energy and apathy
- Changes to appetite (increased or reduced)
- Changes in sleep patterns
- Physical symptoms such as breast swelling, painful joints, and headaches
PMDD can be severe and last until menopause, so treatment is often advisable and necessary to reduce its impact on well-being. Treatment options include anti-inflammatory medicine, selective serotonin reuptake inhibitors (antidepressant medicine), vitamin D, regular exercise, birth control – and professional mental health treatment
Menopause and Depression
This increased risk of depression often starts during perimenopause, which is the stage when estrogen and progesterone levels drop, leading to menopause in women.6 These significant fluctuations in hormone levels can trigger intense mood swings, which can, in turn, increase women’s risk of experiencing depression during menopause. Moreover, women who have gone through periods of depression previously in life may be at increased risk of developing depression during menopause.9
Best Therapy Treatment for Women’s Depression
Depression is a complex illness caused by the interplay between biological, psychological, and environmental factors. For this reason, there is no “one size fits all” approach to mental health.
At Mission Connection, we recognise that an effective treatment plan needs to be tailored to your unique needs. Everyone has different challenges and life stories. Our team of trained professionals can talk you through the best depression treatment options for you, including the following:
Cognitive Behavioral Therapy (CBT)
CBT can help women with depression understand how their thoughts affect their actions, and vice versa. We can help you pinpoint inaccurate thoughts, challenge these, and learn healthy ways to cope with negative emotions and depression.
Trauma-Focused Therapy
Often, our previous experiences, such as trauma, can lead to brain changes and depression. Trauma focused therapy can help you process such experiences in a safe, supportive environment, reducing depression’s impact.
Dialectical Behavior Therapy
DBT was adapted from CBT for people with particularly intense emotions, such as those involved in depression. It can help you address emotional challenges and promote more positive moods and problem-solving skills.
Each of these talk therapies is clinically proven to be effective in treating depression, but they are not the only options we offer. No matter what your mental health concerns, Mission Connection can help, offering you a safe, confidential space to explore challenges and develop healthy coping strategies.
Mission Connection can also provide antidepressant drug therapy, alongside lifestyle management techniques. Staying consistent with therapy, along with any recommended lifestyle modifications and antidepressants, can all lead to the best outcomes for recovery.
When to Seek Support for Depression
If you recognize the symptoms of depression in women in yourself, it’s important to seek professional mental health treatment. Depression can seriously affect emotional and physical health, and these effects can worsen without treatment.
Mission Connection can help. We treat a range of mental health conditions, priding ourselves in our flexible, accessible care for all – alongside bespoke treatment plans. Our licensed therapists are here to support you every step of the way on your journey towards healing and recovery.
If you want to learn more, or have any concerns at all about your mental health, contact us today to find out more about how we can support you on your journey towards recovery.
References
- Salk, R. H., Hyde, J. S., & Abramson, L. Y. (2017). Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychological bulletin, 143(8), 783–822. https://doi.org/10.1037/bul0000102
- Albert P. R. (2015). Why is depression more prevalent in women?. Journal of psychiatry & neuroscience : JPN, 40(4), 219–221. https://doi.org/10.1503/jpn.150205
- National Institute of Mental Health. (n.d.). Major Depression. https://www.nimh.nih.gov/health/statistics/major-depression
- Caputo, J., Pavalko, E. K., & Hardy, M. A. (2016). The Long-Term Effects of Caregiving on Women’s Health and Mortality. Journal of marriage and the family, 78(5), 1382–1398. https://doi.org/10.1111/jomf.12332
- Office for National Statistics. (2019, September 3). Suicides in the UK: 2018 registrations. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/suicidesintheunitedkingdom/2018registrations
- Kundakovic, M., & Rocks, D. (2022). Sex hormone fluctuation and increased female risk for depression and anxiety disorders: From clinical evidence to molecular mechanisms. Frontiers in neuroendocrinology, 66, 101010. https://doi.org/10.1016/j.yfrne.2022.101010
- Psychiatry.org. (n.d.). What is Perinatal Depression? https://www.psychiatry.org/patients-families/peripartum-depression/what-is-peripartum-depression#:~:text=Perinatal%20depression%20refers%20to%20depression,to%20depression%20experienced%20after%20childbirth.)
- Van Niel, M. S., & Payne, J. L. (2020b). Perinatal depression: A review. Cleveland Clinic Journal of Medicine, 87(5), 273–277. https://doi.org/10.3949/ccjm.87a.19054
- Marsh, W. K., Bromberger, J. T., Crawford, S. L., Leung, K., Kravitz, H. M., Randolph, J. F., Joffe, H., & Soares, C. N. (2017). Lifelong estradiol exposure and risk of depressive symptoms during the transition to menopause and postmenopause. Menopause (New York, N.Y.), 24(12), 1351–1359. https://doi.org/10.1097/GME.0000000000000929
Depression in Women FAQs
Women face a combination of biological, psychological, and social factors — including hormonal fluctuations, reproductive events, and higher likelihood of life stressors — that together increase the risk of depression.
Times like puberty, menstruation, pregnancy, postpartum, and perimenopause/menopause are periods when hormonal shifts — paired with life stress or role changes — may heighten vulnerability to depression.
Symptoms may include persistent sadness or low mood, fatigue, sleep or appetite changes, mood swings, loss of interest in activities, difficulty concentrating, and feelings of hopelessness.
Yes. Pressures such as caregiving, work‑life balance, family responsibilities, relational stress, and social expectations can all contribute to depression risk — often interacting with biological and psychological factors.
Because depression in women often arises from a mix of hormonal, social, and emotional factors, a tailored care plan — combining therapy, support, medical oversight, and lifestyle adjustments — ensures treatment addresses the root causes, not just symptoms.
- Signs of Treatment-Resistant Depression
- Signs of Depression Relapse
- Depression-Related Sleep Issues
- Depression Symptom Checklist
- ICD-10 Criteria for Depression
- Major Depressive Disorder (MDD) Symptoms
- Depression Symptoms
- Depression Self-Test
- PHQ-9 Depression Test
- Warning Signs of Depression
- Types of Depression
- Best Therapies for Depression
- Talk Therapy for Depression
- Telehealth for Depression
- Personalized Therapy for Depression
- Holistic Treatment for Depression
- Online Therapy for Depression
- Effective Treatments for Depression
- Medications for Depression
- Treatment-Resistant Depression Options
- Depression Relapse Prevention