Key Takeaways
- CBT with Exposure and Response Prevention (ERP) is considered the gold standard treatment for OCD, with extensive research backing its effectiveness.
- DBT can be particularly helpful for individuals with OCD who also struggle with emotional regulation, intense distress, or have found traditional CBT approaches too confrontational.
- While CBT focuses on changing thoughts and behaviors directly, DBT emphasizes acceptance, mindfulness, and developing coping skills for emotional distress.
- Some individuals benefit from combining elements of both CBT and DBT approaches for comprehensive OCD treatment.
- At Mission Connection, we assess each individual’s unique needs to determine whether CBT, DBT, or a combined approach will offer the most effective treatment path.
OCD Treatment Overview
Deciding on treatment options can be overwhelming when you’re already dealing with the challenges of OCD symptoms. Both Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) offer evidence-based approaches to treating OCD, but they work in fundamentally different ways.
While these therapies share some common elements, they differ significantly in their approach, techniques, and ideal patient profiles. Understanding these differences is crucial for determining which therapy might work best for your specific situation.
What Is OCD?
Obsessive-Compulsive Disorder is characterized by unwanted, intrusive thoughts (obsessions) that trigger significant anxiety, followed by repetitive behaviors or mental acts (compulsions) performed to reduce this distress.
This cycle can become severely debilitating, consuming hours of a person’s day and significantly impairing their quality of life. Common obsessions include fears of contamination, concerns about harm or danger, unwanted sexual or religious thoughts, and needs for symmetry or exactness.
The compulsions that follow these obsessions might include excessive cleaning or handwashing, checking behaviors, counting, arranging items in specific ways, or mental rituals like praying or repeating phrases. What makes OCD particularly challenging is that those who experience it often recognize their thoughts and behaviors as excessive or irrational, yet feel powerless to stop them without experiencing overwhelming anxiety.
Treatment Necessity
Seeking professional treatment for OCD is essential because the disorder rarely improves without intervention. In fact, left untreated, OCD symptoms typically worsen over time as the cycle of obsessions and compulsions becomes more entrenched.
Many people with OCD attempt to manage their symptoms through avoidance or by creating elaborate systems of rituals, but these strategies ultimately strengthen the disorder’s grip on their lives.
Mission Connection offers flexible outpatient care for adults needing more than weekly therapy. Our in-person and telehealth programs include individual, group, and experiential therapy, along with psychiatric care and medication management.
We treat anxiety, depression, trauma, and bipolar disorder using evidence-based approaches like CBT, DBT, mindfulness, and trauma-focused therapies. Designed to fit into daily life, our services provide consistent support without requiring residential care.
CBT for OCD
Cognitive Behavioral Therapy is based on the premise that our thoughts, feelings, and behaviors are interconnected, and by changing unhelpful thought patterns, we can alter our emotional responses and behaviors.
For OCD specifically, CBT helps individuals recognize the connection between their obsessive thoughts and the anxiety that drives compulsive behaviors.
Core Principles
The core principles of CBT for OCD focus on cognitive restructuring and behavioral interventions. It helps individuals understand that intrusive thoughts are a normal part of human experience, but OCD causes an overreaction to these thoughts.
By challenging the meaning assigned to these thoughts, individuals learn they don’t need to engage in compulsive behaviors to manage their anxiety. CBT is directive and goal-oriented, with specific techniques and homework assignments designed to build skills progressively.
ERP Technique
Exposure and Response Prevention (ERP) is the cornerstone of CBT treatment for OCD. This powerful technique involves gradually exposing individuals to situations that trigger their obsessions while preventing them from engaging in their usual compulsive responses.
The “response prevention” component is equally crucial. A therapist supports you in resisting compulsions during and after exposures, which breaks the reinforcement cycle that maintains OCD. This can be incredibly challenging at first, but with practice, you can develop increased tolerance for uncertainty and distress.
Effectiveness Evidence
Research consistently demonstrates that CBT with ERP is highly effective for treating OCD. Studies show that approximately 50–60% of patients who complete a full course of ERP experience significant symptom reduction.
The American Psychological Association, the International OCD Foundation, and other major mental health organizations recognize CBT with ERP as the first-line psychological treatment for OCD based on this robust evidence base.
Treatment Duration
A standard course of CBT for OCD typically ranges from 12–20 weekly sessions, though this can vary based on symptom severity and individual progress. For severe cases, more intensive formats, such as twice-weekly sessions or intensive outpatient programs that provide multiple hours of therapy per week is recommended.
The structured nature of CBT allows for clear treatment goals and timelines, making it easier for individuals to track their progress.
CBT Limitations
Despite its proven effectiveness, CBT for OCD isn’t without limitations. Some individuals find the direct confrontation of fears through ERP too distressing, leading to dropout. Others may have difficulty engaging with the cognitive components if they have limited insight into their thought patterns or struggle with abstract thinking. Additionally, individuals with very severe OCD or multiple comorbid conditions sometimes require more comprehensive treatment approaches.
DBT for OCD
Dialectical Behavior Therapy was originally developed to treat borderline personality disorder but has since been adapted for various conditions, including OCD. While not as extensively studied as CBT for OCD specifically, DBT offers valuable tools that can be particularly beneficial for certain OCD presentations.
DBT’s dialectical framework: balancing acceptance and change offers a gentler entry point for some individuals who find the direct confrontation of ERP overwhelming. Rather than immediately challenging compulsions, DBT first helps individuals develop skills to manage the distress that drives these behaviors.
Mindfulness Focus

Mindfulness in DBT teaches individuals to observe their obsessive thoughts without becoming entangled in them, a skill often described as “watching thoughts float by like leaves on a stream.”
This non-judgmental awareness helps break the automatic reaction of responding to obsessions with compulsions. Individuals learn to recognize that thoughts are just thoughts, not facts or commands that must be acted upon.
Distress Tolerance
Distress tolerance skills are particularly valuable for OCD treatment, as they directly address the anxiety and discomfort that drive compulsive behaviors.
Through DBT, individuals learn concrete techniques to withstand distress without engaging in problematic behaviors. These include self-soothing strategies using the five senses, distraction techniques, improving the moment, and accepting reality as it is rather than fighting against it.
Emotional Regulation
Many individuals with OCD experience intense emotional reactions to their intrusive thoughts, which then fuel compulsive behaviors as attempts to reduce this emotional distress. DBT teaches individuals to identify and label emotions accurately, understand the function of emotions, and reduce vulnerability to emotional suffering.
The DBT concept of “riding the wave” of emotion helps individuals recognize that feelings, no matter how intense, will naturally rise and fall if not amplified by judgments or avoidance. For someone with OCD, this might mean acknowledging the anxiety triggered by an obsessive thought, allowing the feeling to be present without judgment, and watching as it gradually subsides without performing compulsions.
Research Support
While research specifically on DBT for OCD is still emerging, studies have shown promising results for using DBT principles and skills to address symptoms associated with obsessive-compulsive patterns.
Research indicates that mindfulness-based interventions can reduce OCD symptoms like anxiety, stress, and depression by improving awareness of automatic reactions and creating space between thoughts and behaviors.
When DBT Works Best
We’ve found that DBT may be particularly helpful for certain OCD presentations and client profiles. Individuals with significant emotional dysregulation, impulsivity, or self-destructive behaviors alongside their OCD often benefit from DBT’s comprehensive approach to managing these emotional challenges.
Additionally, individuals with comorbid conditions such as borderline personality traits, bipolar disorder, or PTSD may benefit from DBT’s broader approach to emotional management alongside OCD-specific interventions.
Side-by-Side Comparison
| Feature | CBT for OCD | DBT for OCD |
| Primary Focus | Changing thoughts and behaviors directly | Building skills for emotional regulation |
| Key Techniques | Exposure and Response Prevention (ERP), Cognitive Restructuring | Mindfulness, Distress Tolerance, Emotion Regulation |
| Session Structure | Highly structured with specific agenda | Balance of skills training and processing |
| Homework | Exposure exercises, thought records | Skills practice, diary cards |
| Research Support | Extensive research specifically for OCD | Emerging research, stronger for emotional components |
| Best For | Clear obsessions/compulsions, good distress tolerance | Emotional dysregulation, multiple comorbidities |
Combination Benefits
Many individuals benefit from an integrative approach that combines elements of both CBT and DBT. This combined approach provides both the acceptance strategies of DBT and the change-oriented techniques of CBT, addressing both the emotional dysregulation and the specific symptom patterns of OCD.
For example, an individual might first learn mindfulness and distress tolerance skills through DBT modules, then use these skills to support them through increasingly challenging ERP exercises.
Mission Connection: Your Partner in Personalized OCD Treatment
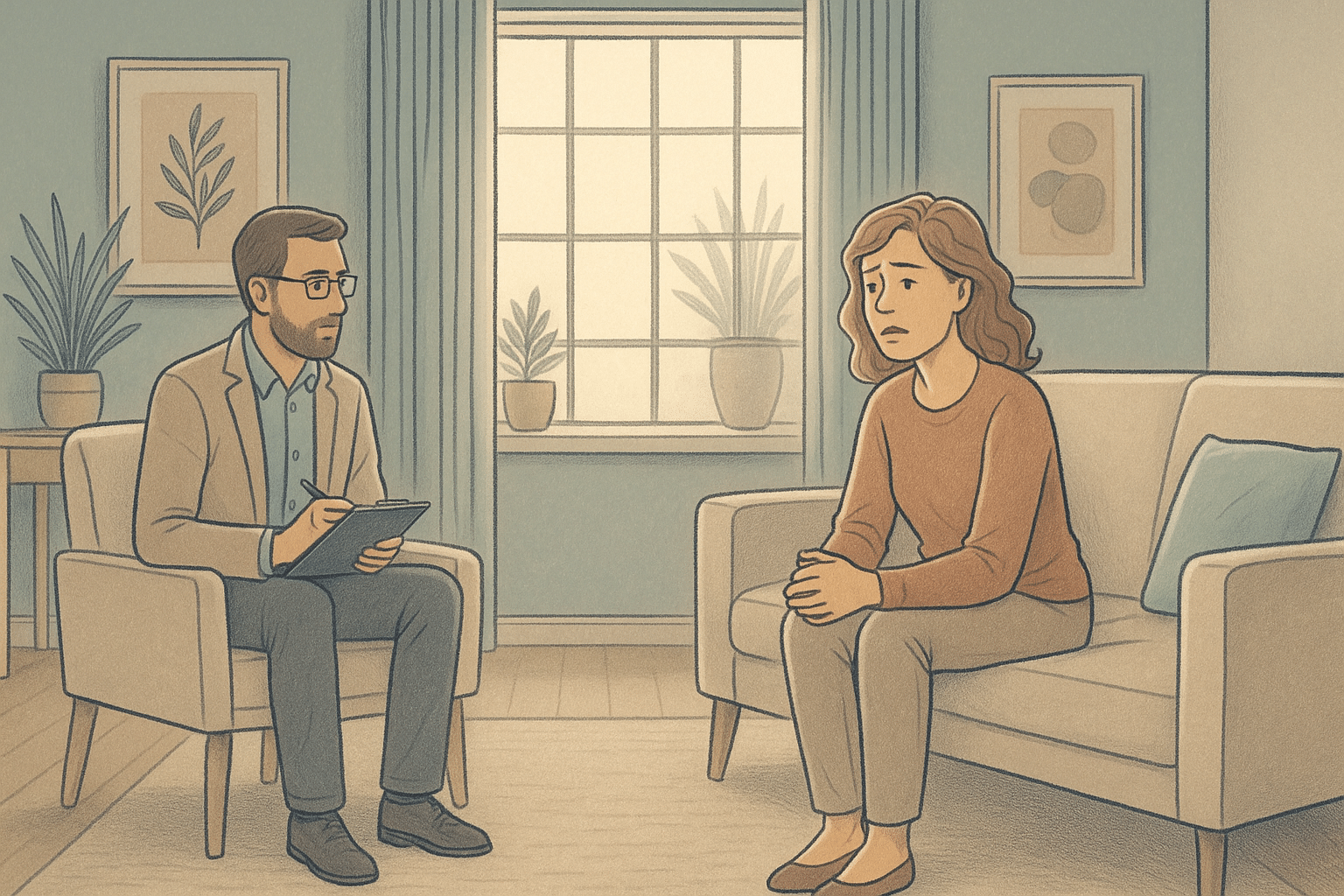
At Mission Connection, our experienced clinical team specializes in both CBT with Exposure and Response Prevention and DBT approaches, allowing us to provide the most appropriate treatment for your specific needs.
We recognize that while CBT with ERP remains the gold standard for OCD, some individuals benefit from the emotional regulation and distress tolerance skills that DBT provides, either as a foundation for later ERP work or as an integrated approach throughout treatment.

What sets Mission Connection apart is our commitment to evidence-based practice combined with individualized care. We conduct thorough assessments to determine whether CBT, DBT, or a combined approach will be most effective for your situation.
Don’t let OCD control your life any longer. Contact Mission Connection today to discover how our personalized, evidence-based approach can help you reclaim your freedom and build lasting recovery.
Call Today 866-833-1822.
Frequently Asked Questions
Is CBT or DBT better for severe OCD?
For severe OCD, the most effective approach is often a combination of medication and intensive therapy. While CBT with ERP has the strongest research support for OCD specifically, severe cases may benefit from starting with DBT skills to build distress tolerance before engaging in challenging exposures.
Does insurance typically cover these therapies?
Most insurance plans cover both CBT and DBT for OCD when delivered by in-network providers, though coverage specifics vary widely. Insurance typically requires a formal OCD diagnosis and may limit the number of sessions or require periodic reviews to confirm medical necessity.
What if neither therapy works for my OCD?
If standard CBT and DBT approaches haven’t provided sufficient relief, treatment-resistant OCD may respond to more intensive interventions, medication adjustments, or innovative approaches. Options include intensive residential treatment programs, Acceptance and Commitment Therapy (ACT), or adjunctive treatments like transcranial magnetic stimulation (TMS).
Can I do both therapies simultaneously?
Rather than pursuing CBT and DBT as separate therapies simultaneously, we recommend an integrated approach that incorporates elements of both. Many skilled OCD therapists draw from both modalities, using DBT skills to support individuals through the challenging process of ERP. At Mission Connection Healthcare, we tailor this integration to each client’s needs, emphasizing different components based on symptom presentation and treatment response so that you receive a cohesive treatment plan.