Key Takeaways
- DBT therapy provides specific skills to manage intense emotions that trigger self-harm, with research showing a reduction in self-harming behaviors.
- The four core DBT skills, mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness, work together to create lasting recovery.
- Distress tolerance techniques like TIPP (temperature, intense exercise, paced breathing, and progressive muscle relaxation) offer immediate alternatives to self-harm during crisis moments.
- DBT’s structured approach includes individual therapy, skills training groups, phone coaching, and a comprehensive safety plan.
- At Mission Connection, we provide specialized DBT therapy programs specifically customized for self-harm recovery, combining evidence-based treatment with compassionate care.
What Self-Harm Really Is
Self-harm, also known as non-suicidal self-injury (NSSI), involves deliberately damaging one’s own body tissue without suicidal intent. Cutting is the most commonly recognized form of self-harm, which encompasses a wide range of behaviors that serve as maladaptive coping mechanisms.
Many people who self-harm report experiencing temporary relief from emotional pain; however, this relief is short-lived and perpetuates a destructive cycle. This behavior is often hidden due to shame and stigma, so it’s important to approach the topic with compassion and understanding rather than judgment.
Mission Connection offers flexible outpatient care for adults needing more than weekly therapy. Our in-person and telehealth programs include individual, group, and experiential therapy, along with psychiatric care and medication management.
We treat anxiety, depression, trauma, and bipolar disorder using evidence-based approaches like CBT, DBT, mindfulness, and trauma-focused therapies. Designed to fit into daily life, our services provide consistent support without requiring residential care.
How DBT Works
Dialectical Behavior Therapy (DBT) works by balancing two seemingly opposite approaches: accepting individuals exactly as they are while simultaneously helping them change harmful behaviors.
This dialectical foundation, the integration of acceptance and change, creates a therapeutic environment where individuals feel understood rather than judged, making them more receptive to learning new coping strategies.
Four Core Skills
The foundation of DBT lies in its four core skill modules, each addressing different aspects of emotional and behavioral regulation. Mindfulness forms the cornerstone, teaching awareness and presence that support all other skills.
Distress tolerance equips individuals with immediate crisis survival strategies when emotions feel unbearable. Emotion regulation helps identify, understand, and change emotional responses. Finally, interpersonal effectiveness enables healthier relationships and boundary-setting.
Evidence of Effectiveness
The research supporting DBT for self-harm is compelling. Multiple randomized controlled trials show significant reductions in self-harming behaviors, with some studies reporting decreases in the frequency of self-injury.
Beyond reducing self-harm, DBT has demonstrated improvements in emotional regulation, distress tolerance, and quality of life.
DBT: Mindfulness Skills
Present Moment Focus
Many individuals who self-harm describe feeling overwhelmed by past traumas or future anxieties. Mindfulness anchors you in the present moment, where you can respond thoughtfully rather than react automatically. Specific techniques like focused breathing, sensory awareness exercises, and mindful observation are used to strengthen this present-moment awareness.
By practicing these skills regularly, even for just a few minutes daily, individuals develop the mental muscles needed to stay present during emotional storms.
Observe Without Judgment
A crucial aspect of mindfulness in DBT is learning to observe thoughts, emotions, and sensations without judging them as good or bad. For individuals who self-harm, harsh self-judgment often triggers or intensifies the urge to self-injure. DBT helps individuals recognize when they’re adding judgmental labels to their experiences and practice describing situations factually instead.
This non-judgmental stance creates space between having a thought like “I’m worthless” and believing it’s true. You learn to recognize such thoughts as temporary mental events rather than facts, reducing their emotional impact and subsequent urges to self-harm.
Daily Practices
Consistent mindfulness practice strengthens the neural pathways that support emotional regulation. We encourage individuals to incorporate brief mindfulness exercises into their daily routines, perhaps while brushing teeth, waiting in line, or before bedtime.
These “mindfulness moments” build the habit of present awareness that becomes accessible during crisis situations.
DBT: Distress Tolerance Techniques
Distress tolerance skills directly address the most urgent need for those who self-harm: managing overwhelming emotions without causing physical damage. These practical techniques help individuals endure distressing situations without making them worse, providing immediate alternatives to self-injury.
Crisis Survival Strategies
When emotional distress peaks and self-harm urges intensify, crisis survival strategies provide immediate relief. These include distraction (engaging in absorbing activities), self-soothing (using the five senses for comfort), improving the moment (finding meaning or encouragement), and evaluating pros and cons of actions.
You can develop personalized crisis plans that incorporate these strategies, customized to your specific triggers and preferences.
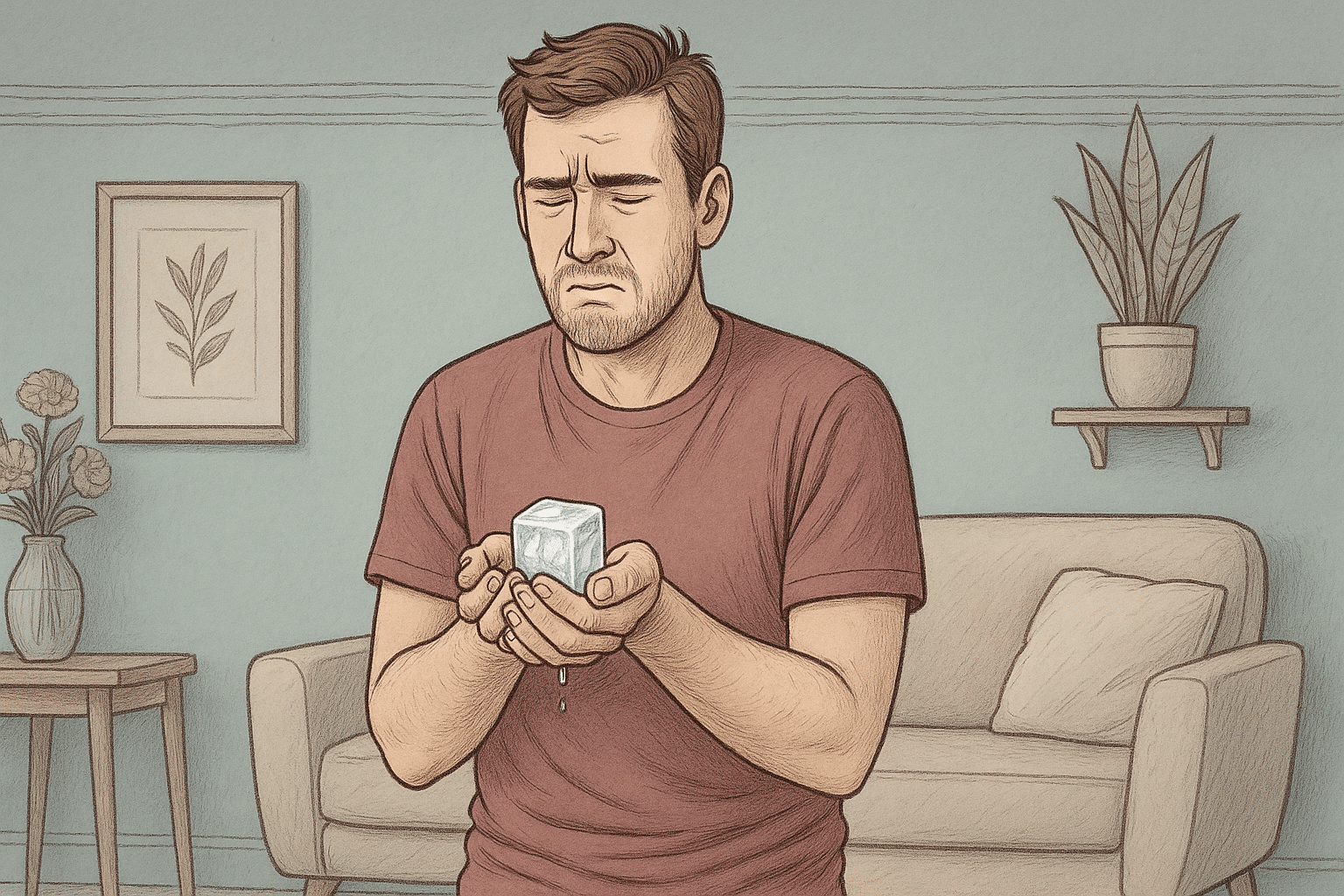
TIPP Skills
The TIPP skills offer powerful physiological interventions that quickly reduce emotional intensity. The acronym TIPP stands for Temperature, Intense exercise, Paced breathing, and Progressive muscle relaxation.
Temperature change (like holding ice or taking a cold shower) activates the mammalian diving reflex, rapidly reducing emotional arousal. Intense exercise burns excess energy and releases endorphins that counter negative emotions. Paced breathing slows the heart rate and activates the parasympathetic nervous system. Progressive muscle relaxation releases physical tension that accompanies emotional distress.
Radical Acceptance
Radical acceptance involves fully accepting reality as it is in the moment, not approving of it, but acknowledging what cannot be immediately changed. For our individuals who self-harm, radical acceptance helps break the cycle of fighting against painful emotions that often leads to self-injury.
This principle teaches that pain is inevitable in life, but suffering is intensified when we fight against reality. By accepting “this is what is happening right now” without judgment, individuals can redirect their energy from resistance to effective response.
DBT: Emotional Regulation
The emotional regulation aspect of DBT teaches individuals to recognize emotions early, understand their functions, and influence their intensity and duration. For those who self-harm, developing these skills reduces the frequency of overwhelming emotional states that trigger self-injury.
Identifying Emotions
Accurately naming emotions is the first step toward managing them effectively. DBT helps individuals develop their emotional vocabulary beyond basic terms like “bad” or “upset,” teaching you to distinguish between sadness, shame, anger, fear, and other primary emotions.
This precision helps identify appropriate coping responses; what works for anger may differ from what helps with shame. You learn to recognize the physical sensations, thoughts, urges, and behaviors associated with different emotions. This awareness allows earlier intervention, before emotions escalate to overwhelming levels that trigger self-harm.
Reducing Vulnerability
The PLEASE skills address physical factors that influence emotional vulnerability: PhysicaL illness (treating promptly), Eating balanced meals, Avoiding mood-altering substances, Sleep hygiene, and Exercise. We emphasize these basics because physical well-being directly impacts emotional resilience.

Creating routines that support these fundamentals provides a foundation for emotional stability.
Building Positive Experiences
Increasing positive emotions builds resilience against self-harm urges. DBT guides individuals to intentionally incorporate activities that generate joy, contentment, interest, and other positive feelings into their daily and weekly routines.
These approaches focus more on creating a balanced emotional life rather than avoiding negative emotions. Over time, this practice expands emotional range and creates alternatives to the relief previously sought through self-injury.
Interpersonal Effectiveness with DBT
The interpersonal effectiveness module teaches concrete skills for expressing needs, setting boundaries, and managing conflicts while maintaining self-respect and relationships. These skills directly address social triggers for self-harm by providing alternatives to the communication function that self-injury sometimes serves.
Setting Boundaries
Many individuals who self-harm struggle with establishing and maintaining personal boundaries, often prioritizing others’ needs at the expense of their own well-being.
DBT teaches specific techniques for identifying boundary violations and communicating limits clearly and respectfully. This reduces resentment and emotional buildup that can lead to self-harm.
DEAR MAN Strategy
The DEAR MAN acronym provides a structured approach to making requests and expressing needs effectively: Describe the situation, Express feelings, Assert wishes, Reinforce positive outcomes, stay Mindful, Appear confident, and Negotiate when needed.
This framework helps individuals communicate clearly in situations where they previously might have suppressed needs and later self-harmed. Role-playing these interactions extensively provides feedback and support for you to develop confidence in your communication abilities.
Self-Respect Building
Maintaining self-respect during interactions represents a crucial aspect of interpersonal effectiveness for those with self-harm histories. Learning to advocate for oneself without excessive apologizing or abandoning personal values builds the self-validation that many individuals lack.
As self-respect grows, the perceived need for self-punishment through self-harm diminishes correspondingly.
DBT Treatment Structure
Individual Therapy
Weekly individual therapy sessions focus on applying DBT skills to specific challenges in the individual’s life, with particular emphasis on reducing self-harming behaviors.
Individual sessions follow a clear hierarchy of priorities: life-threatening behaviors (including self-harm) first, therapy-interfering behaviors second, and quality-of-life issues third. This structure ensures that the most urgent safety concerns receive immediate attention while still working toward broader life goals.
Skills Groups
Weekly skills training groups teach the four core DBT modules in a structured, educational format. These groups typically run for 24–26 weeks, cycling through mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
You learn alongside others facing similar challenges, reducing isolation and providing opportunities to practice skills in a supportive environment.
Phone Coaching
Phone coaching provides brief, focused support between regular sessions when you face crises or struggle to apply skills. This immediate access to coaching helps you implement alternatives to self-harm in the moment when urges arise.
Therapists guide you through specific skills application rather than engaging in extended conversations about the crisis.
Mission Connection’s Commitment to DBT for Self-Harm Recovery

Mission Connection DBT programs are designed for individuals struggling with self-harm behaviors and delivered by clinicians with extensive training in this evidence-based approach. We provide the complete DBT experience through individual therapy, skills groups, phone coaching, and ongoing support, ensuring you have access to help whenever urges arise.
What sets Mission Connection apart is our commitment to making effective treatment accessible through flexible options, including telehealth services, individualized treatment plans, and coordination with your existing support systems. Our approach balances the structure and accountability essential for DBT effectiveness with the understanding and validation you need to heal from self-harm patterns.
Recovery from self-harm is possible, and you don’t have to face this journey alone. Contact Mission Connection today to learn how our specialized DBT programs can help you develop the skills needed to manage overwhelming emotions without self-injury, creating a life worth living beyond mere survival.
Mission Connection offers flexible outpatient care for adults needing more than weekly therapy. Our in-person and telehealth programs include individual, group, and experiential therapy, along with psychiatric care and medication management.
We treat anxiety, depression, trauma, and bipolar disorder using evidence-based approaches like CBT, DBT, mindfulness, and trauma-focused therapies. Designed to fit into daily life, our services provide consistent support without requiring residential care.
Frequently Asked Questions (FAQ)
How long does DBT therapy typically take to reduce self-harm?
Most individuals see initial reductions in self-harm behaviors within the first 3–4 months of comprehensive DBT treatment, though the pace varies individually. Early changes typically include increased awareness of urges, longer delays between urge and action, and use of alternative coping strategies, even if some self-harm continues. Complete resolution of self-harm behaviors generally requires 6–12 months of treatment.
Can DBT work for teenagers who self-harm?
Yes, DBT has been specifically adapted for adolescents who self-harm, with strong research support for its effectiveness. DBT for adolescents (DBT-A) maintains the core components while incorporating developmental considerations, parent involvement, and family skills training.
Is medication needed alongside DBT therapy?
Medication decisions should be made individually based on comprehensive assessment. For some individuals, particularly those with co-occurring conditions like depression, anxiety disorders, or ADHD, appropriate medication can enhance DBT’s effectiveness by reducing symptoms that complicate skill acquisition and implementation. Others may achieve sufficient improvement through DBT alone.
What’s the difference between DBT and CBT for self-harm?
While DBT evolved from Cognitive Behavioral Therapy (CBT) and shares its emphasis on changing thought patterns and behaviors, DBT adds crucial elements specifically relevant to self-harm: dialectical balancing of acceptance and change, extensive focus on emotion regulation skills, mindfulness practices, and validating the individual’s emotional experience. Standard CBT may not sufficiently address the emotional dysregulation and distress tolerance deficits that underlie most self-harming behaviors, making DBT’s specialized approach more effective for these concerns.
How does Mission Connection approach DBT therapy for self-harm?
At Mission Connection, we provide comprehensive DBT programs specifically designed for self-harm recovery. Our experienced clinicians are specifically trained in DBT for self-harm and understand the unique challenges these behaviors present.
We offer flexible treatment options, including telehealth services, to ensure accessibility, and our approach emphasizes creating a safe, non-judgmental environment where individuals feel understood rather than criticized.


