Article-at-a-Glance
- OCD involves persistent unwanted thoughts (obsessions) and repetitive behaviors (compulsions) that cause significant distress and disruption in daily life.
- Common obsessions involve fear of germs, needing things in a specific order, and intrusive thoughts about harm.
- Compulsions may include excessive cleaning, checking, counting, or arranging items.
- Treatment options for OCD include therapy, medication, and self-help strategies to manage symptoms effectively.
- At Mission Connection, we offer comprehensive mental health services for OCD, including professional evaluations, personalized treatment plans, and ongoing support to help you regain control of your life.
OCD Symptom Checklist for Adults
Obsessive-Compulsive Disorder (OCD) is more than being overly tidy or liking things in a certain way—it’s a mental health condition that affects many adults and often causes significant distress and disruption in daily life. If you or someone you know is struggling with OCD, understanding the symptoms is the first step towards managing them.
Common OCD Symptoms
OCD symptoms generally fall into two categories: obsessions and compulsions. Obsessions are intrusive and unwanted thoughts, images, or urges that cause significant anxiety or distress. Compulsions are repetitive behaviors or mental acts that a person feels driven to perform in response to an obsession or based on rigid rules.
Obsessions and Compulsions
Obsessions often revolve around themes such as fear of contamination, needing things to be symmetrical or in a particular order, and intrusive thoughts about harm or taboo subjects. These thoughts can be incredibly distressing, leading to a cycle of compulsions as a way to alleviate the anxiety.
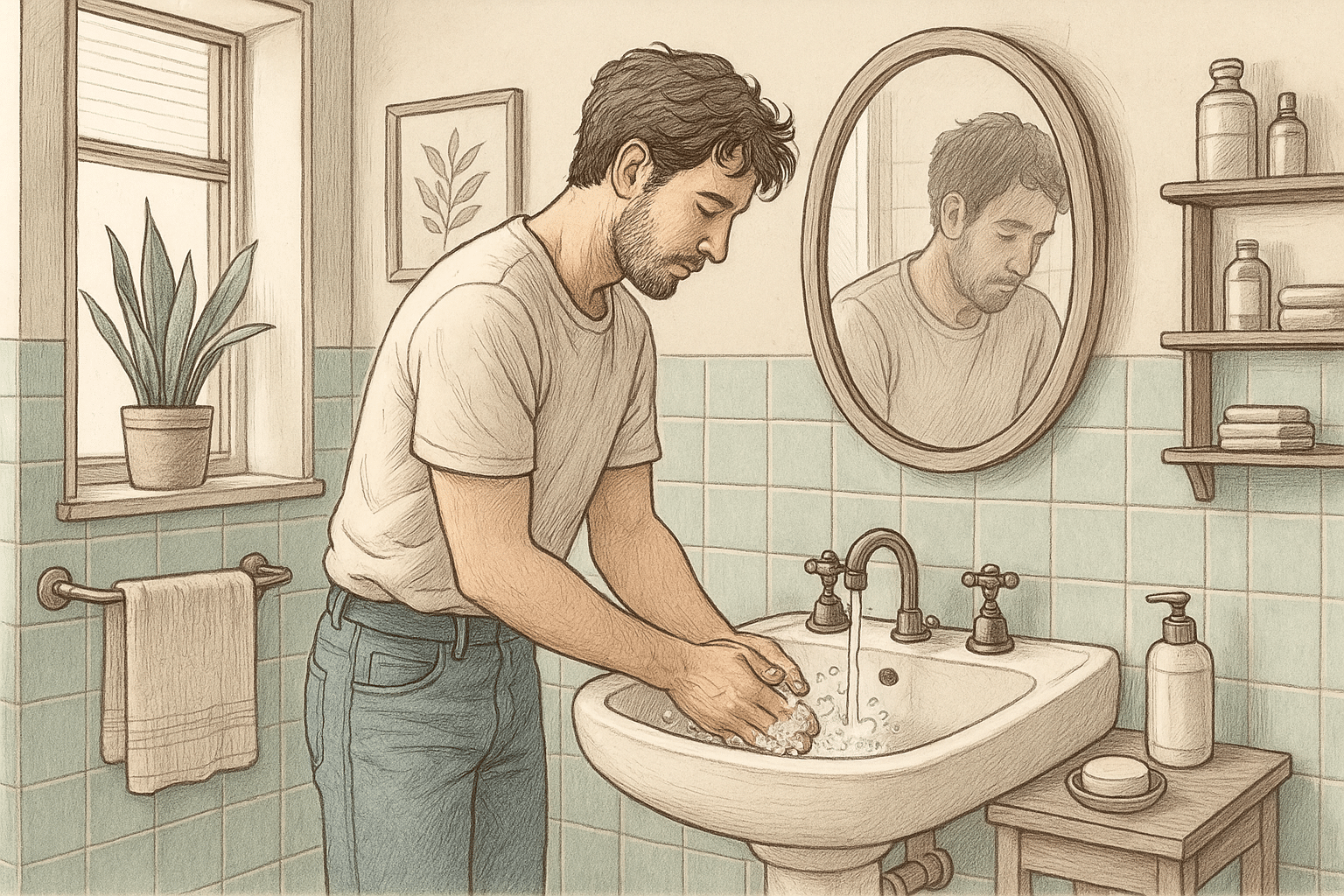
Compulsions are the actions taken to try to prevent or reduce the distress caused by obsessions. For instance, someone with a fear of germs might refuse to shake people or wash their hands repeatedly, sometimes for hours at a time. Another person might check their locks or appliances multiple times before leaving the house.
Impact on Daily Life
The impact of OCD on daily life can be profound. Imagine spending hours each day washing your hands or checking locks, leaving little time for anything else. The constant cycle of obsessions and compulsions can interfere with work, relationships, and social activities, often leading to feelings of isolation or depression.
Beyond that, OCD can create physical symptoms such as fatigue, skin irritation from excessive washing, or headaches from stress. Recognize these symptoms early and seek help to manage them effectively.
Mission Connection offers flexible outpatient care for adults needing more than weekly therapy. Our in-person and telehealth programs include individual, group, and experiential therapy, along with psychiatric care and medication management.
We treat anxiety, depression, trauma, and bipolar disorder using evidence-based approaches like CBT, DBT, mindfulness, and trauma-focused therapies. Designed to fit into daily life, our services provide consistent support without requiring residential care.
Recognizing OCD in Daily Life
Behavioral Indicators
Behavioral indicators of OCD include noticeable rituals or habits that seem excessive or irrational. For example, if you find yourself needing to touch objects a specific number of times or arrange items in a precise manner, these could be signs of OCD. Note that these behaviors are not just preferences but are driven by an overwhelming need to alleviate anxiety.
Emotional Symptoms
Emotionally, OCD can lead to intense feelings of anxiety, guilt, or shame. People with OCD often feel embarrassed about their obsessions and compulsions out of fear of judgment from others. This can lead to avoiding social situations or activities they once enjoyed.
Physical Impact
The stress and anxiety associated with obsessions and compulsions can lead to physical symptoms such as headaches, muscle tension, or stomach issues. Additionally, compulsive behaviors like excessive hand washing can cause skin damage or other health concerns.
Checklist for OCD Severity
Daily Routine Assessment
Assessing your daily routine can help identify patterns and triggers associated with OCD symptoms. Consider keeping a journal to track your activities, thoughts, and feelings throughout the day. This can reveal insights into what exacerbates or alleviates symptoms.
Stress and Trigger Identification
Identifying stressors and triggers is essential for managing OCD. Create a list of situations, people, or environments that trigger obsessions or compulsions. Understanding these triggers can help you develop strategies to manage or avoid them. For more detailed guidance, you might find this OCD symptoms checklist helpful.
For instance, if crowded places increase anxiety, consider planning outings during less busy times.
Keeping Track of Progress
Tracking progress is crucial for recognizing improvements and areas that need more focus. Use a simple chart to record the frequency and intensity of obsessions and compulsions over time. Celebrate small victories since they’re important milestones in managing OCD.
Regularly reviewing this progress with a therapist can provide additional insights and adjustments to treatment plans.
Using the Y-BOCS Rating Scale
The Yale-Brown Obsessive-Compulsive Scale is a 10-item checklist that rates the time spent on obsessions and compulsions, the interference with daily life, the degree of distress, and the success in resisting thoughts and behaviors. This scale helps clinicians understand how severe a person’s OCD symptoms are and guide treatment decisions.
By recognizing and understanding these symptoms, you can take the first steps toward managing OCD effectively. Remember, seeking help from a mental health professional is an important step in finding relief and improving quality of life.
Treatment Options for OCD
Therapy Approaches
Cognitive Behavioral Therapy (CBT) is one of the most effective treatments for OCD. It helps individuals understand the relationship between their thoughts, feelings, and behaviors, providing tools to challenge and change unhelpful patterns. Exposure and Response Prevention (ERP), a type of CBT is another effective option. It involves gradually exposing individuals to their fears while preventing the compulsive response to reduce anxiety over time.
Medications
Medications can be an essential component of OCD treatment, particularly for those with moderate to severe symptoms. Selective serotonin reuptake inhibitors (SSRIs) are commonly used to help balance neurotransmitters in the brain and reduce the intensity of obsessions and compulsions. Work with a healthcare provider to find the right medication and dosage, as this can vary from person to person.
Self-Help Strategies
Grounding techniques such as mindfulness and meditation can help individuals stay grounded and reduce anxiety. Stress management practices, like yoga or deep breathing exercises, can also alleviate symptoms. For example, practicing mindfulness can help individuals become more aware of their thoughts without judgment, reducing the power of obsessions.
Living with OCD
Coping Mechanisms
Developing effective coping mechanisms is crucial for managing OCD symptoms. Techniques such as cognitive restructuring, where you challenge and change unhelpful thoughts, can be beneficial. Additionally, maintaining a healthy lifestyle and engaging in physical activities like exercising might help.
Support Systems
A strong support system can provide encouragement and understanding. Family, friends, and support groups can offer emotional support and practical assistance. Communicate openly with your loved ones about the challenges of OCD, so they can provide the right support.
Building Resilience
Building resilience involves developing the ability to bounce back from setbacks. This can be achieved by setting realistic goals, maintaining a positive outlook, and practicing self-compassion. Resilience helps you manage the ups and downs of living with OCD, fostering a sense of empowerment and control.
Incorporating these strategies into daily life can help you manage your symptoms more effectively and lead a more balanced life. Remember, it’s a journey, and progress is possible with patience and persistence.
Finding Healing With Mission Connection

At Mission Connection, our team specializes in evidence-based treatments for OCD, including CBT with Exposure and Response Prevention (ERP), which has proven highly effective in reducing obsessions and compulsions.
We take a personalized approach to address your specific symptoms and provide tools to manage anxiety and break free from restrictive patterns. Our comprehensive care includes therapy, medication (when appropriate), and ongoing support to help you reclaim your life from OCD.
Don’t let OCD control your daily life any longer. With proper treatment, symptoms can be significantly reduced so that you can focus on what truly matters. Contact Mission Connection today to speak with our compassionate team about OCD treatment options customized to your needs.
Call Today 866-833-1822.
Frequently Asked Questions (FAQ)
How can I distinguish between a habit and OCD?
While habits are regular practices that can be changed with effort, OCD involves persistent, unwanted thoughts and repetitive behaviors driven by anxiety. OCD behaviors are often time-consuming and interfere with daily life, whereas habits are typically less disruptive.
For example, checking the door once before leaving is a habit, but feeling compelled to check it multiple times due to fear of it being unlocked is a sign of OCD.
Is medication necessary for OCD treatment?
Medication is not always necessary for OCD treatment, but it can be beneficial for those with moderate-to-severe symptoms. SSRIs are commonly prescribed to help manage OCD by balancing brain chemicals.
In some cases, therapy alone may be sufficient, especially when combined with self-help strategies and lifestyle changes. The decision to use medication should be made in consultation with a healthcare professional.
What role does family support play in managing OCD?
Family support is crucial in managing OCD. Loved ones can provide emotional support, help identify triggers, and encourage treatment adherence. Open communication about the challenges of OCD can foster understanding and reduce feelings of isolation.
Family members can also assist in creating a supportive environment that minimizes stress and triggers, contributing to more effective symptom management.
How do I approach a loved one I suspect has OCD?
Approaching a loved one you suspect has OCD requires sensitivity and empathy. Start by expressing your concern and willingness to listen without judgment. Create a safe space for them to share their experiences.
Encourage them to seek professional help, but avoid pressuring them. Offer to assist in finding resources or accompany them to appointments if they’re comfortable. Emphasize that OCD is a common and treatable condition, and they’re not alone.
What makes Mission Connection’s approach to OCD treatment effective?
Mission Connection takes a comprehensive approach to OCD treatment, combining evidence-based therapies like CBT and ERP with medication management when appropriate. Our team of experienced mental health professionals creates personalized treatment plans customized to each individual’s specific symptoms and needs so that they’re supported at every step.