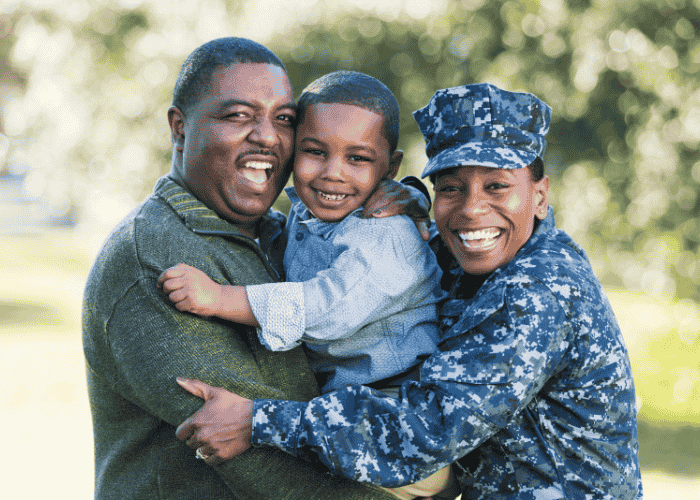
TRICARE Mental Health Coverage for Military & Families

Understanding insurance can be challenging, even in the most stable of times. But when we’re dealing with stress, anxiety, depression, or trauma, it can become even more daunting. Learning the ins and outs of your TRICARE mental health coverage before things become “too much” can alleviate some of the frustration and stress in dealing with insurance.
TRICARE provides benefits for both active-duty and retired service members and their families. But sometimes the benefits aren’t easy to navigate. Coverage can depend on a lot of different factors, like duty status, plan type, and the level of care your doctor recommends. All of which can leave you feeling unsure where to start.
At Mission Connection, we see this confusion every day. If you’re concerned about what your insurance covers, how to verify it, and what your out-of-pocket payments might be, we can help. Our team can walk you through your benefits and how to access treatment that best fits your needs.
This page can also help, as it aims to cover:
- What TRICARE mental health coverage is and the services it usually covers
- What medical necessity means and how TRICARE determines it
- The difference between in-network and out-of-network coverage
- The obstacles you might face when using TRICARE
- Answers to commonly asked questions about TRICARE behavioral health services

What Is TRICARE Mental Health Coverage?
TRICARE mental health coverage is part of the healthcare program for the U.S. military that provides mental and behavioral health support for service members, retirees, and their families.1 It’s not a single insurance plan with one set of rules. It’s a healthcare system that offers multiple options and pathways to care based on your status, location, and type of service.
TRICARE is a health insurance program that combines care through military hospitals and clinics with services contracted from civilian providers. Around nine million people receive care through TRICARE’s network, including routine check-ups, hospitalizations, and specialized mental health treatment.2
In simple terms, this military mental health insurance is meant to ensure that military members and their families can access appropriate behavioral health care. Whether this means talking with a clinician about anxiety, getting evaluated for trauma-related symptoms, or targeting another concern.
What Mental Health Services Does TRICARE Typically Cover?
TRICARE typically covers all mental health services, but the details can differ depending on the type of plan you have and your circumstances. But, essentially, TRICARE is structured to support mental health care across different levels of need, such as:
Outpatient Therapy
TRICARE outpatient mental health treatment is usually where people start, with around 36.2% of people seeking mental health outpatient visits.3 Standard outpatient services usually include weekly or biweekly individual or group therapy, family or couples counseling, and psychiatric services like evaluations and medication. This level of care allows you to get treatment while still being able to continue with regular responsibilities.
Intensive Outpatient Programs
Sometimes we need more than just once or twice a week support. This is where structured outpatient programs can become helpful. TRICARE might cover programs like intensive outpatient (IOP) or partial hospitalization (PHP) when symptoms become more intense.
These programs offer you several hours of therapy for multiple days per week without needing to stay overnight.4 For example, you might attend three hours of IOP per day for four days a week. Or you could attend six hours of PHP a day for five days a week. These TRICARE-covered therapy services offer extra structure while still allowing you to return home at the end of the day.
Inpatient Care
TRICARE inpatient mental health care becomes authorized when safety and stability are concerns. This might look like having severe thoughts of harming yourself or others, experiencing intense hallucinations or delusions, or being unable to care for yourself. These inpatient settings focus on getting you stabilized and making sure you’re safe enough to transition back to outpatient.
Across all levels of care, therapy services address a wide range of mental health concerns, including TRICARE depression treatment, anxiety counseling, and PTSD therapy. Some plans also include TRICARE dual diagnosis coverage when mental health symptoms overlap with other clinical concerns.
What Does Medical Necessity Mean?
The term “medical necessity” often comes up in the exact moment you’re already dealing with so much and trying to get the help you need. And you may interpret it as suggesting that your needs aren’t “enough” for coverage.
The term can sound clinical or impersonal, especially when it determines whether your care is approved or continued. But medical necessity is simply the guide that all insurance companies use to decide what level of care or treatment is appropriate and makes sense for each person’s current needs.
Rather than being a statement about how serious something should be, medical necessity focuses on how symptoms are showing up in daily life. Within TRICARE mental health benefits, this concept helps guide decisions about whether outpatient therapy is sufficient or whether you might benefit from a more structured setting.
How TRICARE Determines Medical Necessity
When TRICARE reviews mental health coverage, decisions are usually made based on the information provided by licensed professionals. This can include the severity of your symptoms, how long they’ve been present, past treatment history, and how you respond to care over time. The process is not about making a judgment about you, but about evaluating the most beneficial treatment as your symptoms improve, change, or become more complex.
For example, you might begin with outpatient mental health treatment and later step into a more structured program if weekly therapy no longer feels like enough. Others may move in the opposite direction, moving back to outpatient care as their symptoms become more stable. These adjustments are part of how TRICARE behavioral health services aim to align care with what’s clinically appropriate in the moment.
The Difference Between In-Network and Out-of-Network
One of the essential parts of any therapy or treatment is the difference between in-network and out-of-network coverage. When using TRICARE mental health coverage, you might wonder whether a provider is covered or not. The following is a breakdown of the distinction.
Working With In-Network Providers
Working with in-network providers often means lower out-of-pocket costs. This is because the provider has an agreement with TRICARE. Starting with an in-network provider is usually more accessible and has fewer administrative steps. Appointments are often easier to schedule, billing tends to be more predictable, and any required approvals are usually handled directly between the provider and TRICARE.
For outpatient care in particular, working in-network can reduce friction and allow people to focus more on treatment itself rather than logistics.
Using Out-of-Network Care
Sometimes you might want to see a provider that is not in-network. Some TRICARE plans allow for this, though each instance could look different. Out-of-network care might make sense if you’re looking for specialized services that aren’t highly available in your area or if you want to continue with a provider you had on another insurance.
But the things to consider when using out-of-network providers are that costs are often higher, reimbursement may only cover part of the fee, or you may need to pay upfront and submit claims afterward. In these cases, TRICARE insurance verification becomes especially important so there are no surprises later.
Understanding the differences between in-network and out-of-network ahead of time can help you make informed decisions about what feels right for you when seeking TRICARE mental health help.
Common Obstacles When Using TRICARE Mental Health Benefits
Even with strong TRICARE mental health benefits in place, many challenges can arise. Many of these come from the systems surrounding the care, rather than the care itself.
One of the most common challenges involves getting the help you want or need immediately. Some insurance plans require referrals for treatment, or providers need to get authorization. These processes can take longer than expected, especially for more specialized treatment, such as inpatient care. When you’re already struggling, waiting around can feel discouraging. This is where TRICARE insurance verification becomes especially crucial, helping you clarify what’s covered and what steps you need to take so there are fewer delays.
Another issue you might encounter is having coverage change over time. Because of medical necessity, approvals for services are reviewed from time to time. This means care may be authorized in phases rather than all at once. While this allows treatment to adjust as your symptoms change, it can also create uncertainty about how long services will continue or what level of care insurance will approve next.
Finally, there’s also the challenge of having to wade through multiple systems at once. TRICARE often works alongside civilian providers, military treatment facilities, and regional contractors. Knowing who handles referrals, billing, or clinical decisions isn’t always obvious, especially if you’re moving frequently or are new to military healthcare.
At every stage of this process, a skilled mental health provider can help you navigate challenges while mitigating concerns.
Finding Support Through TRICARE With Mission Connection
Dealing with insurance at any time can feel complicated, but especially when you’re carrying the weight of military life. Between trying to understand coverage, determining eligibility, and figuring out the next steps, it’s easy to feel stuck before care even begins.
At Mission Connection, we work with you to try to make sense of your TRICARE mental health benefits and explore care options that truly fit your needs. Whether you’re considering therapy, wondering which level of support makes sense, or trying to understand how TRICARE behavioral health services apply to your situation, our team can help walk you through the process with clarity and care.
If you’re ready to take the next step, or even if you’re just looking for answers, we’re here to help you explore your options, verify your coverage, and find a path forward that feels manageable. Reaching out doesn’t have to mean committing to treatment right away. Sometimes it simply means starting a conversation and getting the support you deserve.
Frequently Asked Questions About TRICARE Mental Health Coverage
If you still have some concerns about how to navigate TRICARE mental health coverage after the information in this article, rest assured, you’re not alone. This is why we’ve provided the following answers to FAQs we commonly receive.
Does TRICARE Cover Mental Health Therapy?
Yes, TRICARE mental health coverage includes therapy and other behavioral health services for eligible service members and their families. The specific type of therapy covered and how it’s accessed can vary, which is why understanding your plan details is important.
How Many Sessions Does TRICARE Cover?
The number of sessions TRICARE will cover varies. Your insurance determines this based on medical necessity. They look at factors like how severe your symptoms are, what progress you’re making in current treatment, and what ongoing needs you may have. Your insurance typically reviews treatment over time rather than approves all at once to be able to adjust care as your circumstances change.
Do I Need a Referral to See a Psychiatrist at TRICARE?
Whether you need a referral for a psychiatrist depends on your plan and whether you’re staying in-network or not. For most TRICARE plans, if you are seeing a psychiatrist in-network, you do not need a referral. However, if you decide to go to a TRICARE-approved out-of-network doctor, you may need a referral. According to TRICARE’s website, you don’t need a referral or pre-authorization for outpatient visits, except for psychoanalysis and outpatient therapy for substance use disorder.5
Does Mission Connection Take TRICARE?
We work with a variety of insurance companies to help you get the support you need. If you’re not sure whether our programs accept your insurance, contact us to verify your insurance coverage, and we can walk you through your options. Our goal is to help you understand what types of care may be available to you.
References
- TRICARE. (n.d.). TRICARE 101. https://tricare.mil/Plans/New
- Defense Health Agency. (2024). Evaluation of the TRICARE Program: Fiscal Year 2024 Report access, cost, and quality data through Fiscal Year 2023. In Defense Health Agency. https://www.health.mil/Reference-Center/Reports/2024/09/23/Annual-Evaluation-of-the-TRICARE-Program-FY24
- Germack, H. D., Drake, C., Donohue, J. M., Golberstein, E., & Busch, S. H. (2020). National trends in outpatient mental health service use among adults between 2008 and 2015. Psychiatric Services, 71(11), 1127–1135. https://doi.org/10.1176/appi.ps.201900576
- Zulman, D. M., O’Brien, C. W., Slightam, C., Breland, J. Y., Krauth, D., & Nevedal, A. L. (2018). Engaging High-Need Patients in Intensive Outpatient Programs: A Qualitative synthesis of engagement Strategies. Journal of General Internal Medicine, 33(11), 1937–1944. https://doi.org/10.1007/s11606-018-4608-2
- TRICARE. (n.d.-a). Mental health care appointments. https://tricare.mil/GettingCare/Appointments/MH_Appointments