Disturbing Mental Imagery in Adults: Causes and Signs

Daydreaming, memories, or sudden flashes of imagination are all part of being human. We engage in these without really giving them much thought. Maybe we’re taking a walk in the woods and remembering treading the same path with a grandparent. Or perhaps we’re in a meeting and imagining lying on the beach.
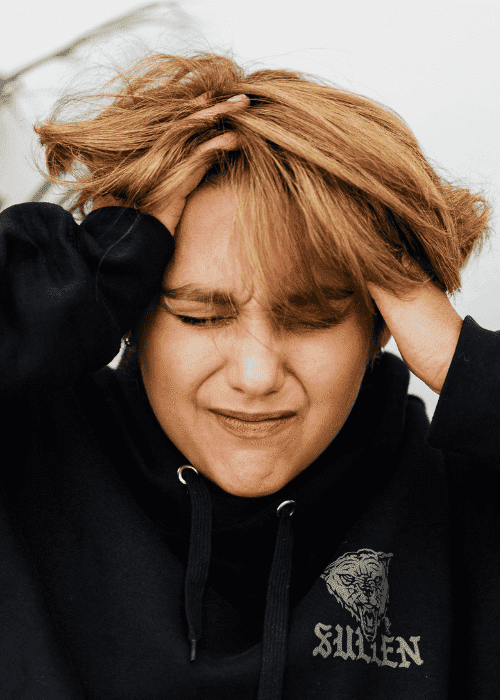
But sometimes, our mental imagery could feel darker and more disturbing. A sudden mental snapshot of a loved one getting hurt. A replay of an accident long after it happened. Scenes such as these can appear out of nowhere and refuse to fade.
These disturbing mental images can feel intrusive – arriving uninvited and bringing up emotions that don’t match the moment. Plus, they can make us feel guilty, confused, or fearful, wondering, Why would I picture something like that?
Intrusive thoughts are surprisingly common, with researchers reporting they affect nearly 94% of us at some point in our lives.1 But if these mental images are consistently disturbing, persistent, and distressing, they might indicate there’s something more going on that you might need to address.
To better help you understand what might be going on, this page will explore:
- How to understand disturbing mental images and the signs you might be experiencing them
- The reasons why intrusive thoughts and images may happen
- Treatment and coping for intrusive thoughts and images
- Where to find professional support
- Answers to commonly asked questions about disturbing mental images
Understanding Disturbing Mental Imagery
Disturbing mental imagery refers to intrusive or unwanted visuals with highly distressing content.2 These images may be memories, flashbacks, or entirely imagined scenes. Though these are only images and not happening in real time, they can still feel very real. Your body may even react to these visuals in a very real way, with the heart racing, muscles tightening, and breathing becoming shallow.
But how can you tell the difference between regular imagination and disturbing mental images?
Signs You May Be Experiencing Disturbing Mental Imagery
Everyone experiences intrusive thoughts and images differently, with many people describing these experiences as feeling like they’re being hijacked by their minds. If you’re not sure whether you’re experiencing disturbing mental imagery, the following descriptions of these visuals may help.
You might have disturbing mental imagery if you’re…
- Having unwanted mental pictures that feel vivid and distressing
- Experiencing repetitive, internal “movies” or mental loops that feel impossible to shut off
- Feeling fearful or guilty about what these images mean, even when you know you won’t act on them
- Avoiding places, objects, or people that trigger the visual memories or thoughts
- Having issues with sleep or nightmares, especially when the images resurface at night
- Find it difficult to concentrate because the mental images intrude
- Consistently seeking reassurance, like checking or confessing to the mental discomfort
- Feeling constantly on alert (hypervigilance), as if the image might become reality
These images don’t necessarily mean you’re experiencing psychosis warning signs. They may just mean you’re experiencing something that’s overloading your nervous system, like unprocessed trauma or unresolved fear.
Why Do Disturbing Mental Images Occur?
Disturbing images don’t just occur out of nowhere. They’re often a reflection of how the brain handles threats. In many cases, our minds use images to express things that words cannot.
Some of the reasons why you might be experiencing intrusive or disturbing mental imagery might be:
Anxiety Disorders
Our imaginations can turn against us when our anxiety is high. For example, the brain may start showing us worst-case scenarios, like images of losing someone, being embarrassed, or being in danger.3 These intrusive imagery anxiety episodes are our minds’ attempt to predict and prevent harm. Though this often ends up worsening the fear instead, creating a feedback loop of fear and anxiety.
Obsessive-Compulsive Disorder (OCD)
Intrusive images are a common feature of obsessive-compulsive disorder, especially harm OCD. In harm OCD, you might experience unwanted thoughts or pictures about harming yourself or others.4 But any type of OCD can cause distressing images.
For instance, with contamination OCD, you might picture yourself covered in germs. And with checking OCD, you might get images of the house being on fire because you didn’t check the stove.
OCD intrusive image symptoms can feel shocking and distressing, and are often in conflict with a person’s values. Plus, if this could be the reason you experience disturbing mental imagery, you might find that trying to hold back or neutralize these visuals often makes them stronger.
Post-Traumatic Stress Disorder (PTSD)
If you have a trauma history, your mind might sometimes replay visual flashbacks of the event as a way to make sense of what happened.5 These PTSD intrusive images may resurface as nightmares or waking flashbacks, triggered by sensory cues that remind the body of past danger.
Psychotic Disorders
Treatment For Intrusive and Disturbing Mental Imagery
When intrusive images start to take up mental space or disrupt daily life, therapy can help you understand what the mind is trying to communicate and how to respond to it with steadier awareness.
Effective approaches for addressing disturbing mental images can include:
Cognitive Behavioral Therapy (CBT) for Intrusive Imagery
CBT is one of the most effective approaches for treating intrusive thoughts and images.7 With CBT for intrusive imagery, you learn how your thoughts, feelings, and body react when these images appear. You can then learn to challenge distorted interpretations, like the belief that imagining harm means you’ll cause it, and then replace those thoughts with a more grounded understanding. Further, CBT often uses something called “imagery rescripting,” in which you revisit distressing images and mentally change the outcome to something more positive.8
Exposure and Response Prevention (ERP)
ERP is highly effective for the treatment of OCD. It’s the practice of confronting thoughts, images, objects, or situations that make you feel anxious and cause distress.9 Basically, when you experience a disturbing mental image, if your normal response is to practice a compulsion, like checking the door is locked ten times, ERP aims to disrupt that response.
Instead of completing the compulsion, when you have a disturbing image, you’ll change your response. For example, by using deep breathing, you may feel capable of sitting with anxiety or worry until it loses its power. With practice, the distress caused by the intrusive thought fades.
Trauma-Focused Therapies
When distressing imagery is a part of trauma, the goal of trauma flashbacks help is to work with the brain to integrate fragmented memories and return to a sense of safety. Trauma-focused interventions include eye movement desensitization and reprocessing (EMDR) and somatic experiencing, which allow the body to process what it may have previously avoided.
EMDR works by using a back-and-forth motion, such as eye movements or tapping (called “bilateral stimulation”) while you think about the distressing image or memory. Experts believe this technique works by activating the brain’s natural ability to heal, similar to what happens during REM sleep.10
Coping With Unwanted Thoughts
Besides engaging in evidence-based therapy, if you encounter disturbing mental imagery, there are some ways you can cope in the moment. For example, you could try:
Grounding in the Present
Bring your senses to your awareness by naming what you can see, touch, or hear. This anchors your body in reality and helps loosen the grip of anxiety and intrusive content.
Shifting the Emotional Charge
Practice mindfulness and deep breathing by taking a slow breath and placing a hand over your heart. Simple gestures like this can calm the body’s alarm system and interrupt the loop between stress and imagination.
Externalizing and Rewriting
Write down or sketch what you see, then change it by altering the ending, softening the colors, or introducing safety or comfort. This kind of mental “rewrite” can help the brain process what once felt threatening and build new associations.
Mission Connection: Professional Intrusive Thoughts Treatment
When your mind begins showing images you never asked to see, it can feel unsettling, like losing control of your own thoughts. At Mission Connection, we help adults understand and manage disturbing mental images through compassionate, evidence-based care. Our clinicians specialize in CBT, EMDR, and exposure therapies to manage intrusive images and take away their power.
If intrusive or distressing images have begun to shape how you feel or function, you don’t have to face them alone. Find support with Mission Connection, as we offer mental health crisis support and ongoing therapeutic care that can help you reconnect to a renewed sense of self.

FAQs About Disturbing Mental Images
If you have some remaining concerns or queries about disturbing mental images, the following responses to commonly asked questions could help you achieve more clarity.
1. Are Disturbing Mental Images Normal?
Yes. Most people experience unwanted images or thoughts from time to time – especially during times of stress, grief, or exhaustion. These moments don’t mean you’re losing control. They usually reflect how the brain processes emotion and threat. When the images become persistent, distressing, or interfere with daily life, it may help to explore them with a therapist.
2. What Causes Disturbing Mental Pictures to Appear?
These images often arise from stress, trauma, or an overactive imagination. Conditions such as anxiety, OCD, or PTSD can heighten the brain’s visual and emotional sensitivity, leading to intrusive imagery anxiety, or PTSD intrusive images. Plus, even without a diagnosis, fatigue, overstimulation, or emotional overload can trigger vivid mental scenes.
3. How Do I Know if I Need Professional Support?
If intrusive imagery causes panic, guilt, or avoidance that affects your sleep, focus, or relationships, you might wonder Would reaching out for a mental health evaluation near me be helpful? The likely answer to this is “yes.” A professional can distinguish between typical intrusive imagery and experiences that may signal something deeper, such as trauma or emerging psychosis warning signs.
4. How Do I Know if These Mental Images Are Part of Psychosis or Not?
The key difference lies in awareness. In most cases of intrusive imagery, you recognize that the images are internal and imagined within your mind, even if they feel vivid or frightening.
However, with psychosis, you may actually believe that the images are real or external, as if they’re happening in the world rather than the mind. If you ever feel unsure, especially if the images seem alive or controlling, it’s important to seek professional guidance right away. Early evaluation can clarify what’s happening and lead to effective support.
5. Does Mission Connection Provide Treatment for Intrusive Imagery?
Yes. Mission Connection offers trauma treatment for adults experiencing distressing or trauma-related mental images. Our team provides compassionate, individualized care, helping you understand what your mind is showing you and how to find calm, clarity, and lasting relief.
References
- Radomsky, A. S., Alcolado, G. M., Abramowitz, J. S., Alonso, P., Belloch, A., Bouvard, M., Clark, D. A., Coles, M. E., Doron, G., Fernández-Álvarez, H., Garcia-Soriano, G., Ghisi, M., Gomez, B., Inozu, M., Moulding, R., Shams, G., Sica, C., Simos, G., & Wong, W. (2013). Part 1—You can run but you can’t hide: Intrusive thoughts on six continents. Journal of Obsessive-Compulsive and Related Disorders, 3(3), 269–279. https://doi.org/10.1016/j.jocrd.2013.09.002
- Brewin, C. R., Gregory, J. D., Lipton, M., & Burgess, N. (2010). Intrusive images in psychological disorders: Characteristics, neural mechanisms, and treatment implications. Psychological Review, 117(1), 210–232. https://doi.org/10.1037/a0018113
- Muse, K., McManus, F., Hackmann, A., Williams, M., & Williams, M. (2010). Intrusive imagery in severe health anxiety: Prevalence, nature and links with memories and maintenance cycles. Behaviour Research and Therapy, 48(8), 792–798. https://doi.org/10.1016/j.brat.2010.05.008
- Gillette, H. (2023, September 20). What is harm OCD? Healthline. https://www.healthline.com/health/ocd/harm-ocd#symptoms
- Bryant, R. A., & Harvey, A. G. (1996). Visual imagery in posttraumatic stress disorder. Journal of Traumatic Stress, 9(3), 613–619. https://doi.org/10.1007/bf02103670
- Allen, S., Goodall, T., Jones, C., James, R., & Surtees, A. (2023). What is the prevalence of visual hallucinations in a First-Episode psychosis population? A systematic review and meta-analysis of the literature. Schizophrenia Bulletin Open, 4(1), sgad002. https://doi.org/10.1093/schizbullopen/sgad002
- Spencer, S. D., Stiede, J. T., Wiese, A. D., Goodman, W. K., Guzick, A. G., & Storch, E. A. (2022). Cognitive-Behavioral Therapy for Obsessive-Compulsive Disorder. Psychiatric Clinics of North America, 46(1), 167–180. https://doi.org/10.1016/j.psc.2022.10.004
- Holmes, E. A., Arntz, A., & Smucker, M. R. (2007). Imagery rescripting in cognitive behaviour therapy: Images, treatment techniques and outcomes. Journal of Behavior Therapy and Experimental Psychiatry, 38(4), 297–305. https://doi.org/10.1016/j.jbtep.2007.10.007
- Hezel, D. M., & Simpson, H. B. (2019). Exposure and response prevention for obsessive-compulsive disorder: A review and new directions. Indian Journal of Psychiatry, 61(7), 85. https://doi.org/10.4103/psychiatry.indianjpsychiatry_516_18
- Stickgold, R. (2008). Sleep-Dependent memory processing and EMDR action. Journal of EMDR Practice and Research, 2(4), 289–299. https://doi.org/10.1891/1933-3196.2.4.289
