Veteran Suicide Prevention: Warning Signs and How to Help

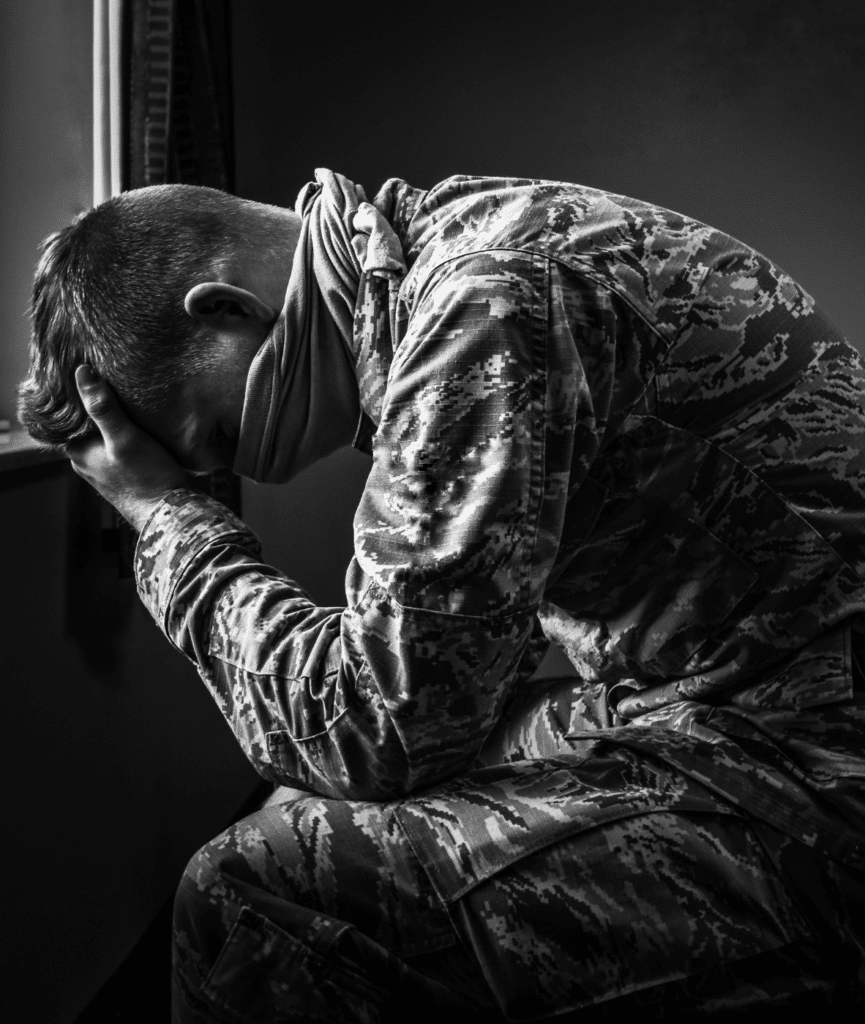
Every day, almost 18 U.S. Veterans die by suicide.1 They aren’t just numbers: they’re people struggling so much that they can’t cope – people like your dad, mom, or partner. For many veterans, transitioning from military to civilian life comes with many challenges, including emotional and mental struggles. Their battle wounds may cut much deeper than they first thought.
Veteran suicide prevention can’t be ignored. You can help recognize the warning signs and offer veterans support, whether you are a friend, family member, or fellow vet. Knowing what signs to look for and what you can do can help save lives.
Mental health awareness for veteran suicide is the first step toward creating lasting change. However, if you’re concerned about your mental health or that of someone you know, reaching out for professional support is important. This guide also covers the essential information about veteran suicide prevention, including:
- What puts Veterans at higher risk of suicide
- Warning signs to look out for
- How you can help a Veteran in crisis
- The role of therapy and peer support in veteran suicide prevention
- Coping strategies for those at risk
Understanding Veteran Suicide
For many Veterans, suicide is a tragic end to an often invisible struggle. According to the U.S. Department of Veterans Affairs (VA) most recent annual report:
- In 2022 alone, there were 6,407 suicides among Veterans. This is almost 18 deaths every day, and it’s 1.5 times higher than the general population1,2
- 73.5% of veteran suicides involve firearms2
- Suicide rates are highest for Veterans aged under 34 years3
- Homeless Veteran suicide rates are especially high, with 84.5 per 100,0003
- The risk of suicide is around 75% higher in veterans who have experienced military sexual trauma3
- LGBTQ+ veterans die by suicide at twice the rate of non-LGBTQ+ veterans3
- Veterans with mental health conditions have an increased risk of suicide3
So why are suicide rates so high in Veterans compared to the general population? Well, there are several things to consider.
One factor is the military experience itself: intense training, combat, life-threatening situations, injury, seeing people you know die in battle…the list goes on. These aren’t experiences that vanish once you leave service – they’re often carried with you through the rest of your life.
Another consideration is the culture change from leaving service and returning to civilian life. A lack of structure or routine, loss of identity, getting used to family, friends, and circumstances that may have changed in your absence, finding employment, and loneliness. Each of these issues can impact mental health.
Mental health disorders are also linked to a higher risk of veteran suicide, especially depression, bipolar disorder, anxiety disorders, and post-traumatic stress disorder (PTSD).2 These conditions can be effectively treated, which highlights the power of getting the right mental health care to prevent suicide.
Additionally, if someone has easy access to firearms, this can increase the risk of suicide, as the majority of suicides in veterans are carried out using this weapon.
These are just a few of the reasons why veterans are at a greater risk of suicide. But remember, suicide is an issue that affects all Americans, including veterans, their families, and their friends. There isn’t always one clear reason for someone taking their life. Veteran suicide prevention is entirely possible with the right help and support.
Warning Signs of Veteran Suicide
For a veteran, accessing the right support before a crisis can be a lifesaver. But sometimes the help and guidance from someone close to them can also make a difference. The warning signs can act as a useful suicide risk assessment for veterans, helping loved ones get them the support they need. Some of the warning signs of suicide in Veterans include:4,5
- Talking about:
- Wanting to die or hurt themselves
- Guilt or shame
- Being a burden to people
- Feeling:
- Hopeless, trapped, or having nothing to live for
- Sad, anxious, agitated, or angry
- Unbearable amounts of pain, either emotional or physical
- Behaviors such as:
- Planning ways to die
- Isolating themselves from friends or family
- Saying goodbyes or giving away their most treasured possessions
- Doing risky things without thinking
- Mood swings
- Sleep problems
- Increase in alcohol or drug use
- Stockpiling medication
As you can tell, some of these signs might be obvious, like giving away possessions or talking about death. But some of them are more subtle, such as bottling up feelings. Knowing the signs to look out for is vital for veteran suicide prevention, so if you recognize any of these in yourself or your loved one, it’s time to seek help.
Helping Veterans at Risk of Suicide
Your loved one is struggling, but what can you do about it? Well, there are a few actions that can really make a difference in crisis intervention for veterans, including the following.
1. Recognize the Signs
You’ve considered the warning signs above and think you notice a few in someone you care about. This is the first step.
2. Choose an Appropriate Time and Place
Think about where to have this sensitive conversation. Perhaps outside while walking, if that’s where they’d feel most comfortable, or at home over a cup of tea. You don’t want children or other people disturbing you mid-way, so somewhere private is best. This way, you can talk about what you’ve noticed and why it has made you concerned.
3. Ask the Question
It’s a question that people can feel highly uncomfortable asking, but it can be a life-saver when it comes to veteran suicide prevention: “Are you thinking of suicide?” You don’t have to phrase it exactly like this. You could try “Are you thinking of killing yourself?” or “Have you been thinking about taking your own life?” Either way, being direct is best – and it won’t put the idea in their head.
However, don’t wait to ask until they are about to leave, or ask in a way that sounds like you’re hoping they say “No.” For instance, saying “You’re not thinking of doing this thing, are you?” may not produce an honest answer.
4. Let Them Talk
You’ve done the hard part: getting the question into the open. They may not be thinking about suicide, but what if they respond that they are? Don’t judge them for what they think or feel at that moment, but recognize that this is a serious situation and that they need help. Be ready to actively listen to and talk with them.
5. Encourage Them to Seek Help
You can help them get the support they need. Reassure them that help is available, and try to get them to immediately seek advice from their doctor, the nearest emergency room, or 911. They could also call the Veterans Crisis Line at 988, option 1, to speak to someone about what they are going through.
6. Keep Them Safe
If you can, stay with them until they get the help they need. You could go with them to their doctor or emergency room, or wait until emergency responders arrive if you have called 911. Make sure that firearms and medicines are safely stored and locked away, as these are some of the most common ways for a person to take their life.
Veteran Suicide Prevention: Therapy and Peer Support
Certain factors can protect against the risk of suicide, which we examine in detail in the following sections.
Preventing Veteran Suicide Through Therapy
As mentioned earlier, certain mental health conditions are linked with a higher risk of suicide in Veterans.2 Yet, by treating mental health challenges such as depression or PTSD with the right support, suicide can be avoided. Therapy can be an effective treatment for many mental health conditions, allowing you the opportunity to explore your thoughts and feelings in a safe space with a professional. These tools help you gain understanding about yourself and learn coping strategies to help you through the tough times. For instance, therapies like cognitive behavioral therapy (CBT) can be effective for treating conditions like depression, anxiety, and even insomnia. Additionally, eye movement desensitization and reprocessing (EMDR) can reduce symptoms of PTSD.
Peer Support for Suicide Prevention
Peer support can be invaluable for veteran suicide prevention. Studies show that peer support allows people to build trusting relationships, which can then reduce loneliness and isolation.6 Veteran peer support also provides understanding, not only of shared mental health challenges, but also of the military culture. Being seen, feeling understood, and forging relationships with peers can go a long way in providing support for veterans at risk of suicide.
VA Suicide Prevention Programs and Resources
The VA has a range of resources geared toward suicide prevention for veterans, including:
- Mental health care
- Local support centers that can connect veterans with services
- Education on how to talk to a veteran in crisis
- Stories of hope and recovery from veterans
- Helplines
- Self-help
- Mobile apps with tools and information
- Access to evidence-based therapies
Coping Strategies for Veterans in Crisis
Mental health challenges and thoughts of suicide can leave someone feeling isolated and hopeless. However, it’s possible to learn coping strategies to help you make it through each day, such as:
- Connecting with people: Talk to loved ones, meet up with friends for a coffee, or attend a peer support group to help remind you that you don’t have to face your struggles alone.
- Mindfulness: Mindfulness can help you feel less stressed, keep you in the present, and allow you to let go of distressing thoughts.
- Distractions: Find a positive distraction you can pour your energy into. For instance, let your feelings and thoughts out into a journal, splash paint on a canvas, or go for a walk with a friend.
- Exercise: Exercise can release endorphins into the system, improving your mood, releasing stress, and burning off adrenaline, all at the same time.
- Routines: Having a good structure in place can be great for your overall mental health. Make a routine covering your basics (like sleep and meal times). Then add in exercise, a hobby, talking to someone, and anything else you think could be helpful.
- Helplines: there are various helplines you can call to talk to someone, 24 hours a day, 7 days a week, including:
- Veterans Crisis Line: Call 988, press option 1.
- Suicide & Crisis Lifeline: Call 988
Don’t hesitate to use any of the suicide prevention resources for veterans mentioned. Reaching out for the help you need shows courage and strength, and early intervention is powerful when it comes to veteran suicide prevention. There is always support available, you only need to ask.
Get Mental Health Support Today
Suicide is preventable, but we know that many people find it difficult to reach out for support. Whether you are struggling with thoughts of suicide or are supporting a loved one through their challenges, we are here to help. We can provide confidential, compassionate, and professional help to support you and your loved one through their crisis.
At Mission Connection, we create a custom treatment plan just for you, based on your needs and goals, because no two people are the same. We offer a range of services including outpatient therapy, medication management, inpatient care, and much more. Cost shouldn’t be a barrier to you getting the help you need, which is why we offer a range of flexible payment options.
We are here to help you on your road to recovery. Ready to take the first step? Contact us today to find out how we can support you.

References
- U.S. Department of Veterans Affairs. (2024, December 19). VA releases 2024 National Veteran Suicide Prevention Annual Report. VA News. Retrieved June 6, 2025, from https://news.va.gov/137221/va-2024-suicide-prevention-annual-report/
- Ruiz, F., Burgo-Black, L., Hunt, S. C., Miller, M., & Spelman, J. F. (2022). A practical review of suicide among Veterans: Preventive and proactive measures for health care institutions and providers. Public Health Reports, 138(2), 223–231. https://doi.org/10.1177/00333549221085240
- U.S. Department of Veterans Affairs. (n.d.). Veteran suicide data and reporting. VA Mental Health. Retrieved June 6, 2025, from https://www.mentalhealth.va.gov/suicide_prevention/data.asp
- National Institute of Mental Health. (2025). Warning signs of suicide [Infographic]. National Institutes of Health. Retrieved June 6, 2025, from https://www.nimh.nih.gov/health/publications/warning-signs-of-suicide
- U.S. Department of Veterans Affairs. (n.d.). Suicide prevention: Prevention. Mental Health. Retrieved June 6, 2025, from https://www.mentalhealth.va.gov/suicide_prevention/prevention/index.asp
- Beehler, S., LoFaro, C., Kreisel, C., Holliman, B. D., & Mohatt, N. V. (2021). Veteran peer suicide prevention: A community‐based peer prevention model. Suicide and Life-Threatening Behavior, 51(2), 358–367. https://onlinelibrary.wiley.com/doi/10.1111/sltb.12712