Key Takeaways
- Intermittent explosive disorder is a recognized mental health condition, not a character flaw. Understanding this can help you respond with compassion rather than frustration.
- During an outburst, staying calm, giving space, and prioritizing safety are more effective than trying to reason with someone in the middle of an episode.
- Setting clear boundaries protects your well-being while still allowing you to support your loved one through their treatment journey.
- Encouraging professional help, particularly therapy-based approaches like cognitive behavioral therapy, is one of the most impactful things you can do.
- Mission Connection Healthcare provides comprehensive, flexible mental health care with individual therapy, group support, and telehealth options designed to help individuals manage IED and related conditions effectively.
Understanding Intermittent Explosive Disorder
Intermittent explosive disorder is a mental health condition characterized by sudden, intense outbursts of anger or aggression that are disproportionate to the situation. These episodes can include verbal outbursts like yelling or heated arguments, or physical aggression such as throwing objects or damaging property. The reactions often seem to come out of nowhere, leaving both the person with IED and those around them feeling confused and distressed.
People with IED typically experience a buildup of tension or irritability before an episode, followed by an explosive release. Afterward, many feel deep regret, shame, or exhaustion. It’s important to recognize that these outbursts are not intentional acts of cruelty or simple bad temper. They represent a genuine difficulty in controlling aggressive impulses, rooted in how the brain processes emotions and regulates behavior.
Living with or caring for someone with IED can feel like walking on eggshells. You may find yourself constantly anticipating the next outburst or struggling to understand what triggers them. The good news is that IED is treatable, and there are practical strategies you can use to support your loved one while also protecting your own mental and emotional health.
Mission Connection offers flexible outpatient care for adults needing more than weekly therapy. Our in-person and telehealth programs include individual, group, and experiential therapy, along with psychiatric care and medication management.
We treat anxiety, depression, trauma, and bipolar disorder using evidence-based approaches like CBT, DBT, mindfulness, and trauma-focused therapies. Designed to fit into daily life, our services provide consistent support without requiring residential care.
5 Strategies for Dealing with Someone with Intermittent Explosive Disorder
1. Stay Calm and Prioritize Safety During Outbursts
When someone with IED is in the middle of an episode, their emotions are running so high that rational conversation becomes nearly impossible. Trying to argue, explain, or correct them at that moment will likely escalate the situation rather than resolve it.
Instead, focus on staying as calm as possible. Keep your voice low and even, avoid making sudden movements, and give the person physical space. Standing at an angle rather than directly in front of them can feel less confrontational. If the situation becomes threatening or you feel unsafe, remove yourself and any children or pets from the area immediately. Your safety always comes first.
Most IED episodes are relatively short, often lasting less than 30 minutes. Sometimes the most helpful thing you can do is simply wait for the intensity to pass before attempting any meaningful dialogue. Once your loved one has calmed down, you can revisit the situation in a more productive way.
2. Learn to Recognize Early Warning Signs
While IED outbursts can feel sudden, there are often subtle warning signs that tension is building. These might include increased irritability, restlessness, clenched fists, pacing, a tightened jaw, or changes in tone of voice. Physical symptoms like a flushed face or rapid breathing can also signal that an episode may be approaching.
By learning to recognize these early cues, you can sometimes help prevent a full-blown outburst. When you notice warning signs, you might gently suggest a break, offer a change of environment, or simply give your loved one space to decompress. Avoid pressing on sensitive topics or demanding immediate responses when tension is high.
This isn’t about tiptoeing around the person or suppressing important conversations indefinitely. It’s about choosing the right moment to engage so that communication can be productive rather than explosive.
3. Set Clear and Healthy Boundaries
Supporting someone with IED does not mean accepting abusive behavior. It’s essential to establish clear boundaries that protect your emotional and physical well-being. Boundaries might include stating that you will leave the room if yelling begins, that certain language is unacceptable, or that you need time apart after an episode to process your own feelings.
Communicate your boundaries calmly and clearly during a peaceful moment, not in the heat of an outburst. Be consistent in enforcing them. Boundaries are not punishments or ultimatums. They are guidelines that allow you to remain supportive without sacrificing your own health and safety.
Setting boundaries also models healthy behavior. It shows your loved one that relationships require mutual respect and that managing their condition is essential for maintaining meaningful connections with the people they care about.
4. Encourage Professional Treatment
One of the most important things you can do for someone with IED is to encourage them to seek professional help. While your support matters, IED is a clinical condition that typically requires structured treatment from mental health professionals.
Cognitive behavioral therapy is one of the most effective approaches for IED. It helps individuals identify the thought patterns and triggers that lead to explosive episodes and teaches healthier ways to respond. Dialectical behavior therapy is another valuable option, focusing on emotional regulation, distress tolerance, and interpersonal skills. Anger management programs can also provide practical tools for recognizing and controlling aggressive impulses before they escalate.
When encouraging treatment, approach the conversation with empathy rather than criticism. Avoid framing it as something they need to “fix” about themselves. Instead, emphasize that treatment can help them feel more in control, reduce the shame and regret that often follow episodes, and improve their relationships and quality of life.
5. Practice Self-Care and Seek Your Own Support
Caring for someone with IED can be emotionally exhausting. The unpredictability of outbursts, the tension of anticipating them, and the emotional aftermath can take a serious toll on your own mental health. It’s not selfish to prioritize your well-being. In fact, it’s necessary.
Make time for activities that help you recharge, whether that’s exercising, spending time with supportive friends, pursuing hobbies, or simply resting. Consider seeking your own therapy or joining a support group for family members of people with mental health conditions. Talking to others who understand what you’re going through can reduce feelings of isolation and provide valuable coping strategies.
Remember that you cannot pour from an empty cup. Taking care of yourself puts you in a better position to offer meaningful support to your loved one over the long term.
What Not to Do When Someone Has an IED Episode
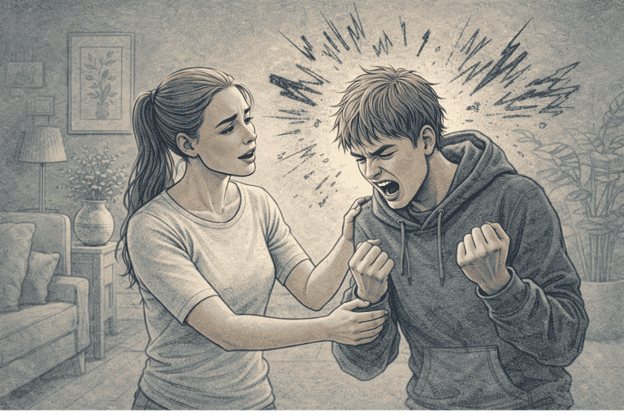
Knowing what to avoid during an outburst is just as important as knowing what to do. Certain responses, though well-intentioned, can make the situation worse.
Avoid arguing or trying to reason with the person mid-episode. Their ability to process logic is significantly impaired when emotions are running high. Raising your voice or matching their intensity will only fuel the fire.
Don’t shame or criticize them during or immediately after an outburst. People with IED often already feel tremendous guilt and embarrassment once an episode passes. Piling on criticism can deepen shame and make them less likely to seek help.
Avoid making threats or issuing ultimatums in the heat of the moment. If boundaries need to be communicated, do so later when everyone is calm.
Finally, don’t ignore your own needs or convince yourself that the behavior is acceptable just because it stems from a mental health condition. Understanding the cause doesn’t mean tolerating harm.
How Therapy Helps People with IED
Therapy is the cornerstone of effective IED treatment. Unlike approaches that simply suppress symptoms, therapy addresses the underlying patterns of thought and behavior that contribute to explosive episodes.
Cognitive behavioral therapy helps individuals recognize the triggers and distorted thinking that precede outbursts. By identifying these patterns, they can learn to interrupt the cycle before it escalates into aggression. Relaxation techniques, such as deep breathing and progressive muscle relaxation, are often incorporated to help manage the physical tension that builds before an episode.
Dialectical behavior therapy offers additional skills for emotional regulation and interpersonal effectiveness. It teaches individuals how to tolerate distress without reacting impulsively and how to communicate their needs in healthier ways.
Anger management programs provide structured environments where individuals can practice new coping strategies, learn problem-solving skills, and develop greater self-awareness. Group settings also offer the benefit of connecting with others who face similar challenges, reducing the isolation that often accompanies IED.
With consistent engagement in therapy, many people with IED experience significant improvement in the frequency and intensity of their episodes, leading to healthier relationships and a better quality of life.
Why Choose Mission Connection Healthcare?

Supporting someone with intermittent explosive disorder is challenging, but you don’t have to navigate it alone. At Mission Connection Healthcare, we understand that IED affects not just the individual but everyone around them. That’s why we offer comprehensive care that addresses the full picture, including anxiety, emotional dysregulation, depression, and the day-to-day struggles that come with managing intense emotions.
Our team of licensed professionals provides personalized treatment plans tailored to each individual’s needs. We offer individual therapy, group support, and psychiatric services, all designed to work together for lasting change. Therapy approaches like cognitive behavioral therapy and dialectical behavior therapy are central to our programs, helping clients build real skills for emotional regulation and healthier relationships.
We also understand that flexibility matters. Our hybrid model includes both in-person sessions and telehealth options, so clients can access care in whatever way works best for their lives. Whether you prefer the structure of face-to-face meetings or the convenience of virtual sessions, we’re here to help.
Mission Connection Healthcare is HIPAA-compliant, insurance-friendly, and available across California, Virginia, and Washington. With daily groups, weekly individual sessions, and access to psychiatric support, everything is designed to be sustainable and effective.
If your loved one is struggling with IED, or if you need support as a caregiver, Mission Connection is ready to help you take the next step toward healing and stability.
Call Today 866-833-1822.
Frequently Asked Questions (FAQ)
Can IED be treated without medication?
Yes, therapy is the primary treatment for IED and can be highly effective on its own. Cognitive behavioral therapy, dialectical behavior therapy, and anger management programs help individuals develop the skills to recognize triggers, manage emotions, and reduce the frequency and intensity of outbursts. Many people experience meaningful improvement through therapy alone.
How long do IED episodes typically last?
Most IED episodes are relatively brief, usually lasting less than 30 minutes. However, the emotional aftermath, including feelings of guilt, shame, or exhaustion, can linger longer. Between episodes, individuals may still experience ongoing irritability or tension.
What should I do if I feel unsafe during an outburst?
Your safety is the top priority. If you feel threatened during an IED episode, remove yourself from the situation immediately. Have a safety plan in place, including a place to go and someone to call. Once the situation has calmed, you can address what happened and discuss boundaries or next steps for treatment.
What types of therapy does Mission Connection Healthcare offer for IED and anger-related conditions?
Mission Connection Healthcare offers individual and group therapy, including cognitive behavioral therapy and dialectical behavior therapy, to help adults and young adults manage IED alongside related concerns like anxiety, depression, and emotional dysregulation.
Our flexible programs include both in-person and telehealth options, along with psychiatric services and daily support groups, so treatment fits into real life while addressing the full range of challenges that come with IED.


